Understanding Parkinson's Core
Parkinson's disease is a relentless neurological condition that affects millions, characterized by the gradual deterioration of specific brain cells responsible
for dopamine production. This neurotransmitter is crucial for smooth motor control, mood regulation, and cognitive functions. As these dopamine-producing neurons diminish, individuals experience symptoms like tremors, rigidity, and slowed movement. In the United States alone, over one million people grapple with Parkinson's, with approximately 90,000 new diagnoses occurring annually. Current medical interventions can alleviate symptoms but do not halt the disease's progression, underscoring the urgent need for restorative therapies. This pioneering research shifts focus from symptom management to addressing the fundamental cellular deficit, offering a potential pathway to disease modification.
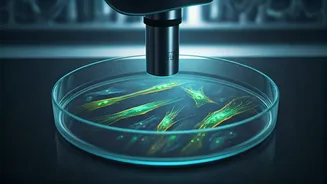
Innovative Stem Cell Approach
A significant advancement in Parkinson's research involves a clinical trial examining the efficacy of specially engineered stem cells. These induced pluripotent stem cells (iPSCs), derived from adult cells like skin or blood, are reprogrammed into a versatile state, capable of differentiating into various cell types. The critical aspect is their directed differentiation into dopamine-producing brain cells. This therapeutic strategy aims to directly replace the neurons lost to Parkinson's, thereby restoring the brain's natural dopamine levels. By implanting these iPSCs into the basal ganglia, a brain region vital for motor control, researchers hope to re-establish disrupted neural circuits. This approach offers a unique potential to not only alleviate motor deficits but also potentially slow or even reverse the disease's underlying pathology, offering a proactive solution rather than reactive symptom management.
The Surgical Procedure
The implantation of these specialized stem cells is a meticulously planned surgical procedure. Under the precise guidance of magnetic resonance imaging (MRI), neurosurgeons create a small opening in the patient's skull to access the basal ganglia. This region, central to regulating movement, is the target for stem cell delivery. The iPSCs are then carefully injected into this area. Following the surgery, patients undergo an intensive monitoring period, typically spanning 12 to 15 months. This observation phase is critical for evaluating the treatment's safety and effectiveness, specifically looking for any improvements in Parkinson's symptoms and potential side effects such as involuntary movements (dyskinesia) or infection. Long-term follow-up, extending up to five years, allows for a comprehensive assessment of the treatment's enduring impact on motor function and overall quality of life.
Trial Scope and Goals
This groundbreaking clinical trial is a collaborative effort, with Keck Medicine of USC participating alongside two other institutions in the United States. The study is designed to assess the safety and potential efficacy of this novel stem cell therapy in individuals with moderate to moderate-severe Parkinson's disease. A total of 12 participants are enrolled in this multisite endeavor. The overarching aspiration of this research is to pioneer a reproducible technique that can effectively repair motor function compromised by Parkinson's disease. By doing so, the ultimate goal is to significantly enhance the quality of life for patients, offering them a renewed sense of control over their movements and daily activities. This trial represents a significant step towards potentially offering a restorative treatment for a condition that has long been managed rather than cured.