Understanding Ayushman Bharat
The Ayushman Bharat scheme, officially PM Jan Arogya Yojana (PMJAY), represents a monumental stride in India's healthcare landscape. Launched in 2018,
it aims to provide significant financial protection against catastrophic health expenditures for the country's most vulnerable populations. As the world's largest government-funded healthcare initiative, PMJAY targets over 10 crore families, encompassing both rural and urban poor, offering a substantial insurance cover of ₹5 lakh per family annually. This plan subsumes the earlier Rashtriya Swasthya Bima Yojana (RSBY) and is designed to be an entitlement-based system, ensuring that beneficiaries can access medical and hospitalisation services without financial burden. The scheme has already facilitated millions of hospital admissions, demonstrating its impact on improving healthcare access and affordability across India. Its operational commencement in September 2018 marked a new era in public health, with a focus on secondary and tertiary care, making quality medical treatment more accessible to a vast segment of the population.
Who is Covered?
Ayushman Bharat (PMJAY) is meticulously designed to support families identified through the Socio-Economic Caste Census (SECC) of 2011, focusing on those facing deprivation and specific occupational challenges. The scheme extends its reach to approximately 50 crore individuals, encompassing 8.03 crore rural families and 2.33 crore urban families. A key feature is the absence of any restrictions on family size or age, ensuring that all members, including women, children, and the elderly, are protected. The entitlement is determined by specific criteria within the SECC database. For rural areas, these criteria include families residing in single-room dwellings with basic structures, those lacking an adult member between 16 and 59 years, female-headed households without a prime-age adult male, families with disabled members and no able-bodied adult, SC/ST households, and landless labourers. Additionally, households without shelter, destitute individuals, those living on alms, manual scavengers, primitive tribal groups, and legally released bonded labourers are automatically included. In urban settings, entitlement is based on 11 defined occupational categories, such as beggars, rag-pickers, domestic workers, street vendors, construction workers, sanitation staff, home-based workers, transport workers, shop assistants, mechanics, washer-men, and chowkidars. Beneficiaries of the Rashtriya Swasthya Bima Yojana (RSBY) in active states also remain eligible.
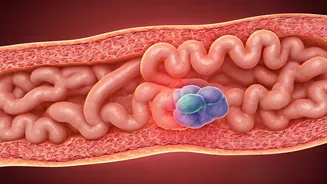
Accessing Benefits and Treatment
For beneficiaries, the Ayushman Bharat scheme operates on a cashless and paperless system, eliminating financial barriers to healthcare. There are no charges or premiums for hospitalisation expenses, and the benefits extend to cover pre- and post-hospitalisation costs. Each empanelled hospital is equipped with an 'Ayushman Mitra' to guide patients, manage documentation, verify eligibility, and facilitate enrollment. Upon arrival at a hospital, beneficiaries will present a letter with a QR code, which is scanned for demographic authentication to confirm eligibility. The scheme's provisions are portable, allowing beneficiaries to receive cashless treatment at any public or empanelled private hospital nationwide. The scheme covers a wide array of medical and hospitalisation expenses, encompassing nearly all secondary and most tertiary care procedures. Over 1,354 treatment packages are included, offering services like coronary bypass surgery and knee replacements at rates often lower than those under the Central Government Health Scheme (CGHS). Hospitals wishing to be empanelled generally require a minimum of 10 beds, though states can adjust this. Empanelment is managed through an online portal, and information on these facilities is readily available via government websites and mobile apps. For assistance, beneficiaries can contact the helpline at 14555. Treatment costs are managed through pre-defined package rates, with potential incentives for accredited hospitals.
Eligibility and Application Process
It is crucial to understand that Ayushman Bharat (PMJAY) is an entitlement-based scheme, meaning there is no active application or enrollment process for individuals to join if they are not already identified. Eligibility is strictly determined by the government based on the SECC 2011 data, using the outlined deprivation and occupational criteria for rural and urban populations, respectively. Families whose names appear on the official SECC list are automatically entitled to the scheme's benefits. Lists of eligible families have been shared with state governments and their respective departments for dissemination. While new families cannot be added, existing eligible families can include additional members if their names are on the SECC list. Families holding an active RSBY card as of February 28, 2018, are also covered. Beneficiaries can verify their eligibility and find lists of empanelled hospitals on the official Ayushman Bharat PMJAY website, www.abnhpm.gov.in. The scheme ensures that those who qualify can access essential healthcare services without financial strain, thereby fulfilling its objective of providing universal health coverage to the underprivileged sections of society.