Cervical cancer develops in the cells of the cervix, the lower part of the uterus that connects to the vagina. Traditionally, it has been considered a disease affecting women in their late 40s or older.
However, over the past decade, doctors have increasingly been diagnosing cervical cancer and precancerous changes in much younger women, including those in their 20s and 30s.
India continues to have one of the highest burdens of cervical cancer globally, accounting for nearly one-fourth of worldwide cases. While the overall numbers remain high, a worrying trend is the shift toward younger age groups. This is largely due to lifestyle changes, early HPV exposure, and low screening rates. Unlike many cancers, cervical cancer develops slowly, offering a critical window for early detection yet this opportunity is often missed in younger women.
Why Are Younger Women at Risk Today?
The primary cause of cervical cancer is persistent infection with high-risk strains of the Human Papillomavirus (HPV). Today, younger women are being exposed to HPV earlier in life, increasing the risk of cervical cellular changes at a younger age.
Key contributing factors include:
Early onset of sexual activity
Multiple sexual partners or a partner with multiple contacts
Smoking, which weakens local immunity
Poor nutritional status and a weakened immune system
Lack of regular cervical screening
Many young women believe cervical cancer is “too early” for them, leading to delayed Pap smears and missed detection of cervical dysplasia, the silent precancerous stage that can progress if left untreated.
Symptoms and Warning Signs Often Ignored
One of the biggest challenges with cervical cancer is that the early stages often show no symptoms at all. When symptoms do appear, they are frequently subtle and mistaken for routine gynaecological issues.
Warning signs to watch for include:
Irregular or abnormal vaginal bleeding
Bleeding after intercourse
Persistent foul-smelling or unusual vaginal discharge
Pelvic pain or discomfort
Younger women often ignore these symptoms, assuming they are stress-related or hormonal. Unfortunately, this delay can allow the disease to progress to advanced stages, where treatment becomes more complex.
Who Is More Prone to Developing Cervical Cancer Early?
Certain groups of women are at higher risk and require closer monitoring.
High-risk groups include:
Sexually active women under 40 who have never been screened
Women who assume HPV vaccination eliminates all risk
Those with compromised immunity
Women with a history of long-term oral contraceptive use
Individuals with limited access to preventive healthcare
A common misconception is that HPV vaccination removes the need for screening. While vaccination is highly protective, it does not cover all cancer-causing HPV strains, making regular screening equally essential.
Prevention, Screening, and Treatment: What Can Be Done
The most powerful tools against cervical cancer are prevention and early detection.
Key preventive and management strategies include:
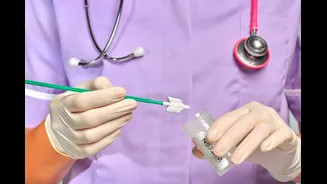
Regular Pap smears and HPV testing as advised
HPV vaccination for eligible age groups
Early treatment of cervical dysplasia before it becomes cancerous
Stage-appropriate treatment options such as surgery, radiation, or chemotherapy
When detected early, cervical cancer has a very high cure rate. Timely consultation with a gynaecologist ensures that abnormal changes are addressed before they become life-threatening.
Conclusion: Early Awareness Can Save Young Lives
Cervical cancer is no longer a disease limited to older women. The rising number of cases among younger women highlights the urgent need for awareness, routine screening, and proactive healthcare behaviour.
Every woman regardless of age should prioritise cervical health, understand the importance of regular check-ups, and seek medical advice for any unusual symptoms. Early action not only saves lives but also preserves long-term health, fertility, and quality of life.