Inflammation is increasingly emerging as a common underlying factor in many modern health and fertility challenges. “At a population level, inflammation is becoming a common thread running through several
fertility-related concerns,” says Dr Shivika Gupta, Fertility Specialist at Birla Fertility & IVF, Gurgaon. “It can be described as a double-edged sword, while it protects the body against infection, maintains homeostasis and repairs tissue damage, chronic inflammation can damage cells and tissues and even contribute to autoimmune disease.”
Understanding Acute and Chronic Inflammation
According to Dr Gupta, inflammation exists in two forms: acute and chronic. “Acute inflammation is protective and short-lived,” she explains. “However, when it does not resolve and persists for long periods, it develops into chronic low-grade inflammation.”
This form of inflammation is a continuous, low-intensity process that can gradually harm the body. It is often driven by metabolic stress, poor sleep, sedentary lifestyles, chronic psychological stress and diets high in ultra-processed foods. Over time, it can alter how the body uses energy, regulates hormones and maintains cellular health.
Why Fatigue and Weight Gain May Signal Inflammation
“One of the earliest signs people notice is persistent fatigue,” says Dr Gupta. “Inflammatory signalling interferes with mitochondrial function, the process by which cells produce energy leaving individuals feeling constantly drained, even when routine blood tests appear normal.”
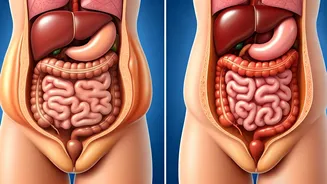
Inflammation also affects metabolic health. “It disrupts insulin sensitivity and encourages fat accumulation, particularly around the abdomen,” she explains. “This further reinforces the inflammatory cycle and makes weight management more challenging.”
Impact on Overall Health and Fertility
Chronic inflammation has been linked to the development and progression of serious medical conditions, including ulcerative colitis, cardiovascular diseases, endometriosis and certain cancers.
“One of the less recognised consequences of chronic inflammation is its impact on reproductive health, particularly female fertility,” Dr Gupta notes. “It can influence hormone regulation, egg quality, ovulation and the uterine environment, ultimately reducing the chances of successful implantation.”
Effects on Male Reproductive Health
The impact is not limited to women. “In men, sustained inflammation increases oxidative stress within the testes,” says Dr Gupta. “This can damage sperm membranes and DNA, leading to reduced sperm count, poor motility and increased DNA fragmentation.”
She adds that these changes are increasingly being observed even in younger men without obvious reproductive disorders, highlighting the widespread effects of chronic inflammation.
Managing Inflammation for Better Reproductive Health
From a fertility perspective, addressing inflammation plays a crucial role in improving overall reproductive outcomes. “Managing inflammation is not an alternative to assisted reproductive treatments, it is an essential foundation for them,” Dr Gupta explains.
She recommends adopting lifestyle habits that support metabolic and inflammatory health. “Regular physical activity, adequate sleep, stress management and a balanced diet rich in whole foods, fibre, fruits, vegetables and healthy fats can help reduce chronic inflammation,” she says.
“When metabolic and inflammatory health are optimised, reproductive treatments are more likely to work with the body rather than against it,” concludes Dr Gupta.