Stage 1: Steatosis Begins
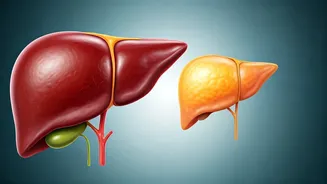
The initial phase of fatty liver disease is known as Steatosis, or mild fatty liver. This stage is characterized by an accumulation of fat within the liver cells.
Typically, in Steatosis, the liver can become enlarged, but it often functions normally. This stage is frequently asymptomatic, meaning that there are no noticeable symptoms. As a result, many people remain unaware they have the condition. Diagnosing Steatosis often involves blood tests that reveal elevated liver enzyme levels, and imaging tests like ultrasounds can also help in detection. Lifestyle adjustments such as dietary changes and increased physical activity can frequently reverse the effects of Steatosis and prevent further progression. Early intervention is key, as managing this stage effectively can significantly reduce the risk of developing more severe liver conditions.
Stage 2: NASH Emerges
Non-alcoholic Steatohepatitis (NASH) marks the second stage of fatty liver disease. NASH is a more serious condition than Steatosis, as it involves inflammation and liver cell damage. This stage can lead to fibrosis, the formation of scar tissue in the liver. Individuals with NASH may experience fatigue, abdominal pain, and unexplained weight loss. NASH can be more challenging to detect than Steatosis since it requires more advanced testing, such as a liver biopsy. The progression to NASH increases the risk of developing severe complications like cirrhosis and liver failure. Lifestyle changes become crucial at this stage, and medical interventions, including medications, may be necessary to manage the inflammation and protect the liver from further damage. Effective management involves a multidisciplinary approach focusing on diet, exercise, and medical supervision.
Stage 3: Liver Fibrosis Develops
Stage 3 of fatty liver disease involves liver fibrosis, where significant scarring occurs. This scarring results from prolonged inflammation and damage to the liver cells, often stemming from unresolved NASH. As fibrosis progresses, the liver's ability to function properly is compromised. Symptoms may become more noticeable, including jaundice (yellowing of the skin and eyes), swelling in the abdomen (ascites), and easy bruising. At this stage, the liver is still capable of regeneration, but the damage is more extensive and the risk of developing cirrhosis increases. Treatment focuses on managing the underlying causes, such as diabetes and obesity, alongside medications to control inflammation and potentially slow the progression of fibrosis. Regular monitoring and advanced medical care are essential to prevent the disease from advancing to the final stage.
Stage 4: Cirrhosis Happens
The final stage of fatty liver disease is cirrhosis, a severe condition characterized by extensive, irreversible scarring of the liver. The liver becomes severely damaged and unable to function correctly, leading to a cascade of life-threatening complications. Symptoms include severe jaundice, ascites, internal bleeding, and hepatic encephalopathy (brain dysfunction). Cirrhosis can result in liver failure, increasing the need for a liver transplant. Managing cirrhosis involves intensive medical care, including treating the complications that arise, such as fluid retention and bleeding. While cirrhosis is irreversible, early detection and aggressive management can improve the quality of life and potentially extend the lifespan by slowing the disease progression. Liver transplantation may become necessary if liver failure develops.