What is PsA?
Psoriatic arthritis (PsA) is a chronic inflammatory disease that impacts both the skin and the joints. It is closely associated with psoriasis, a skin condition
marked by scaly, itchy patches. PsA is a type of arthritis that affects individuals with psoriasis, and it can cause pain, swelling, and stiffness in the joints. Understanding PsA involves recognizing its connection to psoriasis and the varied ways it can manifest, influencing both skin and joint health. The presence of psoriasis is a key factor, making the diagnosis of PsA more likely. Recognizing and managing this condition can involve a combined approach to address both skin and joint symptoms effectively.
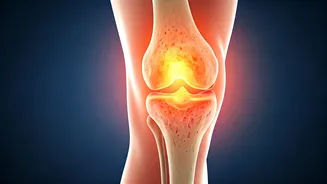
PsA: Key Symptoms
The symptoms of psoriatic arthritis vary greatly from person to person, often mirroring the variability of psoriasis itself. Common symptoms include pain, swelling, and stiffness in the joints, particularly in the fingers and toes. Sometimes, this can lead to dactylitis, where entire fingers or toes swell up. Other symptoms include skin changes like psoriasis plaques, nail problems such as pitting or separation, and eye inflammation. Fatigue and a general feeling of being unwell are also frequently reported. The extent and severity of symptoms can fluctuate over time. This can cause periods of flares and remissions. Early recognition of these signs is essential for early diagnosis.
PsA: Potential Causes
The exact causes of psoriatic arthritis are not fully understood, but it's believed to be a combination of genetic, environmental, and immune system factors. Genetics play a significant role, with certain genes increasing the risk of developing the condition. Environmental triggers, such as infections or injuries, may activate the immune system in susceptible individuals. The immune system mistakenly attacks the body's tissues, leading to inflammation in the joints and skin. Research indicates that an overactive immune response is a main factor. This knowledge helps in devising treatment plans aimed at suppressing the immune system and reducing inflammation.
PsA: Types Explained
Psoriatic arthritis can manifest in various forms, each characterized by distinct patterns of joint involvement. The most common type is asymmetric arthritis, which affects different joints on each side of the body. Another type is symmetric arthritis, which mirrors the symptoms of rheumatoid arthritis. Distal interphalangeal predominant PsA involves the small joints of the fingers and toes, often accompanied by nail changes. Spondylitis-predominant PsA primarily affects the spine, leading to back pain and stiffness. Finally, arthritis mutilans is a severe form that results in significant joint damage and deformity. Recognizing these varying forms is crucial for tailored management plans.
PsA: Treatment Options
Effective management of psoriatic arthritis usually includes a combination of medication, lifestyle adjustments, and therapies. Medications play a key role in reducing inflammation and slowing disease progression. These might include nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, disease-modifying antirheumatic drugs (DMARDs), and biologics. Physical therapy can improve joint mobility and reduce pain. Regular exercise and a balanced diet are also important for managing symptoms and maintaining overall health. Additionally, lifestyle modifications like stress management and avoiding triggers can help control flares. Regular monitoring by a healthcare professional is important to adjust treatments and ensure the best possible outcomes.
Early Diagnosis Matters
Early diagnosis of psoriatic arthritis is crucial for preventing joint damage and improving long-term outcomes. Because PsA can overlap with other types of arthritis, it may be a challenge to diagnose. Early detection can lead to timely intervention, which helps prevent irreversible joint damage and improve overall quality of life. Diagnosis typically involves a combination of a physical examination, medical history review, and imaging tests like X-rays or MRIs. Blood tests are used to rule out other conditions. If you experience joint pain, stiffness, or skin changes associated with psoriasis, consult a healthcare professional. Early treatment can help you to manage PsA effectively.
PsA vs. Other Arthritis
Distinguishing psoriatic arthritis from other types of arthritis is important because each condition requires a specific approach to management. Unlike rheumatoid arthritis, PsA often has a more variable pattern of joint involvement, frequently affecting the fingers and toes. The presence of psoriasis and nail changes is a key indicator. Osteoarthritis, on the other hand, is a degenerative disease related to wear and tear on the joints, and it doesn’t typically include skin or nail problems. Diagnosing PsA requires a thorough evaluation, taking into account the unique combination of joint and skin symptoms. By accurately identifying PsA, clinicians can deliver targeted treatments that address its specific characteristics.