Disrupting Gut Flora
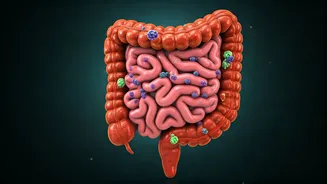
Antibiotics, while effective against bacterial infections, can inadvertently harm the beneficial bacteria residing in your gut. These 'good' bacteria play
a crucial role in digestion, nutrient absorption, and immune function. The broad-spectrum nature of many antibiotics means they cannot distinguish between harmful and helpful bacteria. This indiscriminate action can lead to a significant reduction in the diversity and population of these beneficial microorganisms. This imbalance, often referred to as dysbiosis, can have wide-ranging consequences for overall health, setting the stage for various digestive issues and potentially increasing susceptibility to other health problems. The gut's microbial ecosystem, a complex network of bacteria, fungi, and viruses, needs to maintain a delicate balance for optimal health, which antibiotics can severely disrupt.
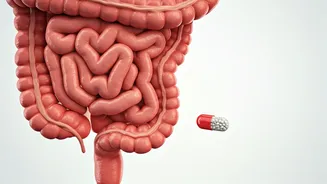
Causing Antibiotic-Associated Diarrhea
One of the most common side effects of antibiotic use is antibiotic-associated diarrhea (AAD). This occurs because antibiotics disrupt the natural balance of bacteria in the gut, allowing harmful bacteria, such as Clostridioides difficile (C. diff), to overgrow. C. diff infections are particularly dangerous and can cause severe diarrhea, abdominal pain, and fever. In some cases, AAD can lead to dehydration and other serious complications, requiring immediate medical attention. The severity of AAD can vary from mild, self-limiting episodes to severe, life-threatening conditions. Proactive measures, such as taking probiotics, may help to mitigate the risk of AAD, but it is always best to consult a healthcare professional.
Increased Risk of Infections
The use of antibiotics can weaken the gut's defenses, making individuals more susceptible to various infections. The gut microbiome plays a crucial role in preventing the colonization of harmful pathogens. When antibiotics disrupt the microbial balance, it creates an environment where these pathogens can thrive. This increased susceptibility extends beyond the gut, potentially affecting other areas of the body. Infections such as yeast overgrowth (candidiasis) are common side effects of antibiotic use. Furthermore, long-term antibiotic use can lead to a weakened immune response, increasing the risk of both bacterial and viral infections. Protecting your gut health is thus essential in maintaining overall immunity and warding off infections.
Impaired Nutrient Absorption
A healthy gut microbiome is essential for efficient nutrient absorption. The beneficial bacteria in the gut help break down complex carbohydrates and other nutrients, making them accessible to the body. Antibiotics can negatively impact this process by reducing the population of beneficial bacteria. This can lead to malabsorption of essential nutrients such as vitamins, minerals, and fatty acids. This deficiency can cause fatigue, weakness, and other health problems. Long-term use of antibiotics can lead to a chronic state of malabsorption, impacting overall health and well-being. It is important to replenish gut health with probiotics and nutrient-rich foods after antibiotic treatment to restore proper absorption.
Developing Antibiotic Resistance
One of the most concerning consequences of antibiotic misuse is the development of antibiotic resistance. When antibiotics are used excessively or inappropriately, bacteria can adapt and become resistant to the drugs. This means that future infections caused by these resistant bacteria will be harder, and sometimes impossible, to treat. This is a growing global health crisis. Antibiotic resistance poses a serious threat to public health. Proper antibiotic stewardship involves using antibiotics only when necessary and in the correct dosage to minimize the risk of developing resistance. Educating the public about the importance of responsible antibiotic use is crucial to combating this growing challenge.
Impact on Immunity
The gut microbiome significantly influences the immune system. A balanced gut microbiome helps regulate immune responses, protecting against infections and preventing autoimmune diseases. By disrupting the balance of gut bacteria, antibiotics can impair immune function. This can lead to a weakened immune system, making individuals more susceptible to infections. It may also increase the risk of developing autoimmune disorders, where the immune system attacks the body's tissues. The gut is often considered the 'gateway' to the immune system. Preserving gut health is essential to maintaining a strong immune defense and overall health.
Inflammation and Gut Issues
Antibiotics can contribute to increased inflammation in the gut, which can lead to various digestive problems. Disruption of the gut microbiome can trigger an inflammatory response. This inflammation can cause symptoms like abdominal pain, bloating, and changes in bowel habits. In some cases, prolonged inflammation can lead to chronic gut conditions. Conditions such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) can worsen. Maintaining a healthy gut environment through a balanced diet, probiotic supplements, and limiting unnecessary antibiotic use is crucial to managing inflammation. Early detection and treatment can help prevent long-term complications.
Altering Gut Metabolism
The gut microbiome plays a vital role in metabolism. The gut bacteria help break down food, extract energy, and produce various metabolic byproducts. Antibiotics can disrupt this metabolic activity by altering the composition of the gut microbiota. This can affect how the body processes carbohydrates, fats, and other nutrients. These alterations can have widespread effects on health, potentially influencing weight management, blood sugar control, and other metabolic processes. Changes in the gut microbiome can increase the risk of developing metabolic disorders. Restoring gut health is essential to restoring healthy metabolic functions and overall well-being.
Impact on Mental Health
Emerging research reveals a strong connection between gut health and mental well-being, often called the gut-brain axis. The gut microbiome influences brain function through various pathways. Antibiotics, by disrupting the gut microbiome, can indirectly impact mental health. This can potentially contribute to mood disorders like anxiety and depression. Gut bacteria produce neurotransmitters, such as serotonin and dopamine. These neurotransmitters are essential for regulating mood. The imbalance caused by antibiotics can disrupt this process. Studies suggest that maintaining a healthy gut microbiome can positively affect mental health and overall cognitive function. Addressing gut health is, therefore, crucial in supporting both physical and mental wellness.
Long-Term Consequences
The effects of antibiotic misuse can have long-lasting consequences for gut health. While the gut microbiome can often recover after antibiotic use, the process is not always complete. Repeated or prolonged use of antibiotics can cause lasting changes in the gut environment. This could lead to chronic digestive problems and increase the risk of developing various health conditions. In extreme cases, the gut microbiome may never fully recover its original composition and functionality. Proper care, including probiotic supplementation and dietary changes, can help mitigate these long-term effects. A proactive approach towards gut health can support long-term digestive and overall well-being.