What's Happening?
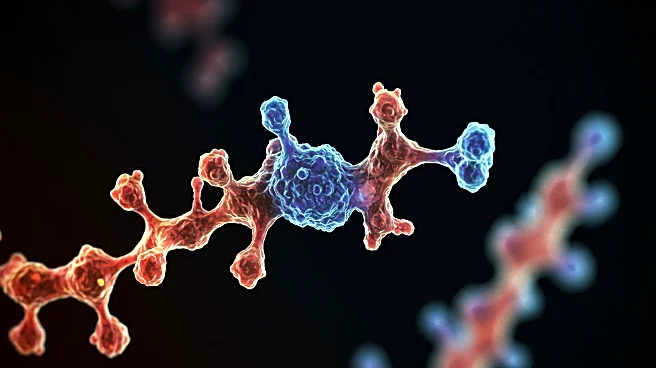
Recent research has focused on the genetic modification of human pluripotent stem cells (hPSCs) to reduce immune cell adhesion, specifically targeting the ICAM-1 protein. The study involved knocking out ICAM-1 in hPSC-derived cardiovascular therapies, including cardiomyocytes, endothelial cells, and cardiac fibroblasts. This genetic modification resulted in significantly diminished binding of multiple immune cell types, suggesting potential hypoimmune properties. The research utilized CRISPR technology to edit stem cell lines, aiming to inhibit immune cell binding and reduce immune response in stem cell therapies. The study was conducted under the approval of the University of Wisconsin's Institutional Review Board and Animal Care and Use Committee, ensuring compliance with federal and state laws.
Why It's Important?
The findings of this study have significant implications for the field of regenerative medicine and stem cell therapy. By reducing immune cell adhesion, the modified stem cells could potentially evade immune detection, leading to improved outcomes in stem cell-based treatments. This could benefit patients requiring cardiovascular therapies, as the risk of immune rejection is a major challenge in stem cell transplantation. The research opens avenues for developing hypoimmune stem cell lines that could be used in various therapeutic applications, potentially reducing the need for immunosuppressive drugs and enhancing the safety and efficacy of stem cell therapies.
What's Next?
Future research will likely focus on further refining the genetic modifications to enhance the hypoimmune properties of stem cells. Clinical trials may be initiated to test the safety and effectiveness of these modified stem cells in human patients. Additionally, researchers may explore the application of this technology to other types of stem cell therapies beyond cardiovascular treatments. Stakeholders, including medical professionals and biotech companies, will be closely monitoring these developments to assess the potential for commercialization and integration into existing treatment protocols.
Beyond the Headlines
The ethical implications of genetically modifying stem cells to evade immune detection are significant. While the potential benefits are substantial, concerns about long-term effects and unforeseen consequences must be addressed. The research also highlights the growing role of CRISPR technology in medical advancements, raising questions about the regulation and oversight of genetic editing in clinical settings. As the technology progresses, discussions around ethical guidelines and patient consent will become increasingly important.