What's Happening?
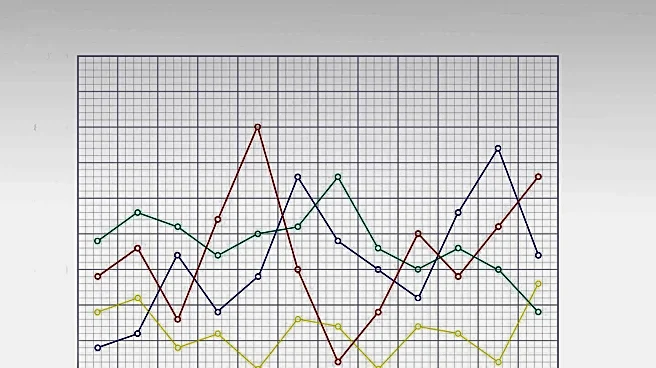
A new predictive nomogram model has been developed to differentiate between benign and malignant pancreatic masses. This model uses individual symptoms such as anorexia and weight loss, along with routine laboratory values like blood type, CA19-9, and IgG4, to provide a visual means for predicting clinical outcomes. The nomogram aims to improve the precision of clinical predictions and contribute to the risk stratification of diseases, thereby enhancing patient management. The study involved 494 patients, making it one of the larger sample sizes in this field, and demonstrated a higher ability to differentiate between benign and malignant pancreatic masses compared to previous models.
Why It's Important?
The development of this nomogram is significant as it offers a simple, cost-effective, and widely accessible tool for diagnosing malignant pancreatic masses. This can facilitate early clinical decision-making and timely referral, especially in primary care settings where advanced imaging modalities may not be accessible. The model's inclusion of blood type as a predictive factor is novel and highlights the potential biological mechanisms linking ABO blood groups to pancreatic cancer risk. By providing a practical tool for early differentiation, the nomogram could improve patient outcomes and reduce the burden of invasive testing.
What's Next?
The study suggests that further rigorous external validation in different centers is necessary before clinical implementation to ensure the generalizability and clinical benefits of this model. The nomogram is intended to complement existing screening tools and diagnostic methods, not replace them. Continuous monitoring and rigorous follow-up are recommended for patients identified as low risk, while those at moderate or high risk should be referred for further imaging and biopsy.
Beyond the Headlines
The study emphasizes the importance of age stratification in predicting pancreatic malignancy, noting that older patients have a higher likelihood of malignant masses. This suggests that early detection programs could be particularly beneficial for reducing pancreatic cancer mortality in older populations.