What's Happening?
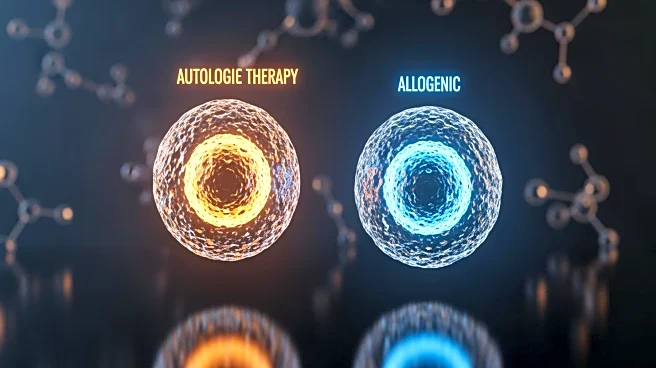
A groundbreaking case has emerged where a man with type 1 diabetes has successfully produced his own insulin following a gene-edited cell transplant. This procedure, detailed in the New England Journal of Medicine, involved transplanting genetically modified islet cells that were engineered to evade the immune system's rejection. The transplant, conducted by scientists from Sweden and the U.S., marks the first human application of this technique. The patient has been able to produce insulin without the need for immunosuppressive drugs, which are typically required to prevent organ rejection.
Why It's Important?
This development represents a potential breakthrough in diabetes treatment, offering hope for a long-term solution to insulin dependency. By using CRISPR technology to modify donor cells, the risk of immune rejection is minimized, potentially eliminating the need for lifelong immunosuppressive therapy. This approach could revolutionize the management of type 1 diabetes, improving quality of life and reducing healthcare costs associated with the disease. If successful in further trials, this method could pave the way for similar treatments for other autoimmune conditions.
What's Next?
Researchers plan to conduct follow-up studies to assess the long-term viability of the transplanted cells and their ability to produce insulin over time. Further testing will determine the approach's effectiveness in a broader patient population. Success in these areas could lead to widespread adoption of gene-edited cell transplants as a standard treatment for type 1 diabetes.