Understanding Atrial Fibrillation
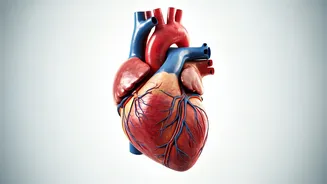
Atrial fibrillation, or AFib, is a condition characterized by an irregular and often excessively rapid heartbeat, medically classified as an arrhythmia.
This chaotic rhythm prevents the upper chambers of the heart, the atria, from beating in a coordinated manner, leading to inefficient blood flow into the lower chambers, the ventricles. This inefficiency can cause blood to pool and form clots within the heart. These clots pose a severe threat, as they can dislodge and travel to vital organs, most notably the brain, significantly elevating the risk of a stroke. In fact, individuals with AFib face a five-fold greater chance of experiencing a stroke compared to those with a regular heart rhythm. AFib episodes can be transient, occurring intermittently, or they can become a persistent, chronic condition. The implications of AFib are stark; the mortality rate where it's identified as a primary or contributing factor has been on an upward trend for over two decades. In the United States, over 454,000 individuals are hospitalized annually due to AFib, with a tragic outcome of 158,000 deaths. Projections indicate a further escalation, with an estimated 12.1 million Americans expected to be diagnosed with AFib by the year 2050.
Recognizing AFib Symptoms
When atrial fibrillation strikes, it often manifests through a range of noticeable symptoms. A common experience is palpitations, which can feel like a racing heart, a pounding sensation, fluttering, or the unsettling feeling of skipped beats. Beyond these direct heart sensations, individuals might also experience chest discomfort or pain. Physical exertion can become more challenging, leading to a decreased ability to exercise. Fatigue or a general sense of tiredness is also frequently reported, alongside shortness of breath. Dizziness or a feeling of faintness can occur, highlighting the potential impact on circulation and overall well-being. While these symptoms can vary in intensity and frequency, their presence warrants medical attention to rule out or diagnose AFib and its potential consequences.
Who Faces AFib Risk?
Several factors can increase an individual's susceptibility to developing atrial fibrillation. As age advances, the risk of AFib tends to climb. Pre-existing health conditions also play a significant role, including high blood pressure, heart failure, and ischemic heart disease. Other medical issues like diabetes, hyperthyroidism, and chronic kidney disease are also linked to a higher likelihood of AFib. Lifestyle choices contribute substantially; moderate to heavy alcohol consumption and smoking are identified risk factors. Genetic predisposition may also be a factor, with European ancestry noted as a risk indicator. Furthermore, conditions such as obesity and an enlarged left side of the heart can predispose individuals to AFib. In some instances, external triggers can precipitate AFib episodes, including the consumption of alcohol, caffeine, recreational drugs, experiencing emotional stress, or even consuming spicy foods.
Strategies for Heart Health
To proactively protect your heart and minimize the risk of developing AFib and experiencing strokes, experts emphasize a multi-faceted approach. A fundamental recommendation is to abstain from smoking and all forms of tobacco use. Engaging in regular physical activity is crucial; aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous activity per week, or a combination of both. Nourishing your body with a heart-healthy diet is paramount, which includes prioritizing fiber-rich foods, nuts, and fish, while consciously limiting salt and saturated fat intake. Maintaining a healthy body weight is also essential for cardiovascular well-being. Prioritizing quality sleep and effectively managing stress levels contribute significantly to overall heart health. Finally, regular health screenings are vital for early detection and management of any underlying conditions that could impact your heart.