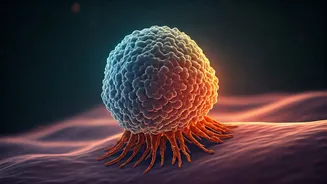
Immune Cell Allies
The remarkable potential of the human immune system to combat cancer is being actively explored. A significant focus lies on leveraging immune cells located
within tumors themselves. Scientists have recognized that these cells, specifically macrophages, can be re-engineered to become potent anti-cancer agents. These modified macrophages, often referred to as 'CAR-macrophages,' are designed to target and destroy cancer cells. This approach marks a significant shift in cancer therapy, moving beyond traditional methods to harness the body's natural defenses to directly attack tumors from within, creating a significant impact in treatment strategies.
CAR-macrophage Strategy
The development of CAR-macrophages involves a sophisticated process. Macrophages are reprogrammed to express Chimeric Antigen Receptors (CARs) on their surface. These CARs are specifically designed to recognize and bind to antigens present on cancer cells. Once the CAR-macrophage identifies a cancer cell, it binds to the antigen and initiates an immune response, leading to the destruction of the targeted cancer cell. This targeted approach is intended to provide greater precision compared to conventional therapies, potentially reducing harm to healthy cells. This highlights an approach where personalized medicine is becoming a reality in the realm of cancer treatment.
Therapy Challenges Faced
Despite the promise, cancer therapy, particularly the use of CAR-macrophages, faces significant challenges. One of the main hurdles is the complex nature of the tumor microenvironment, especially in solid tumors. These solid tumors create a protective shield that hinders immune cell infiltration and function. Another challenge includes the development of strategies to overcome these obstacles and ensure that CAR-macrophages can effectively reach and eliminate cancer cells within the complex tumor landscape. Addressing these challenges is crucial for the effective translation of these promising therapies into clinical success, paving the way for more effective treatments.
Treatment Hurdles Explored
Current CAR-macrophage therapies have limitations. Researchers are working to enhance the efficacy of these therapies by improving macrophage trafficking, persistence, and anti-tumor activity within solid tumors. Strategies also include optimizing CAR design to ensure efficient cancer cell recognition and killing. Furthermore, scientists are exploring combination therapies, where CAR-macrophages are used together with other cancer treatments to enhance their effects. Overcoming these hurdles is paramount to developing therapies that can provide better outcomes for patients with solid tumors and other forms of cancer, making the current therapies more promising.
Reprogramming Techniques Used
A critical aspect of CAR-macrophage therapy is the reprogramming of macrophages. Scientists are employing cutting-edge techniques, including the use of lipid nanoparticles, to efficiently introduce the necessary genetic modifications into the macrophages. Lipid nanoparticles are used to deliver the genetic material that encodes the CARs into macrophages. Once inside the cells, the genetic material is expressed, leading to the production of CARs on the macrophage surface, thereby converting the cells into potent cancer fighters. This innovative method represents a substantial improvement in the ability to reprogram immune cells for therapeutic purposes.
Study Findings Unveiled
The latest studies have shown promising results in pre-clinical models, showing how CAR-macrophages can effectively target and destroy cancer cells. The studies highlight the potential of these therapies to overcome some of the challenges associated with solid tumors. The findings provide valuable insights into optimizing CAR design, improving macrophage persistence, and enhancing overall anti-tumor activity. These results pave the way for clinical trials to evaluate the safety and efficacy of CAR-macrophage therapies in patients, representing a step closer to turning laboratory breakthroughs into real-world cancer treatments.