Urbanization and Allergies
Urban environments are often cited as hotspots for increased allergy prevalence, and sinus allergies are a significant example of this. Several intertwined
elements contribute to this phenomenon, starting with the air quality. Cities frequently grapple with higher levels of air pollutants, encompassing particulate matter from vehicle exhaust, industrial emissions, and construction activities. These contaminants can directly irritate the nasal passages and mucous membranes, causing inflammation. Furthermore, these pollutants can also act as carriers for allergens, like pollen and mold spores, making their entry and impact more severe. This constant assault on the respiratory system can lead to the overactivation of the immune system, leading to the development and worsening of allergies. In essence, the concentrated air pollutants and allergens found in urban areas set the stage for a heightened allergic response, leading to a rise in sinus allergy cases.
Air Pollution’s Role
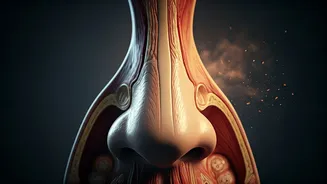
A significant factor driving the increase in sinus allergies within cities is the presence of air pollution. The composition of urban air, with its cocktail of particulate matter, noxious gases, and chemical compounds, has a direct impact on the respiratory system. These pollutants can inflame the nasal passages, causing them to become more sensitive to allergens. Moreover, air pollution can act as an adjuvant, which boosts the immune response to other allergens. When the body encounters both pollutants and allergens simultaneously, the immune system is significantly triggered, amplifying allergic reactions. The sustained exposure to polluted air, frequently seen in urban centers, chronically irritates the nasal and sinus tissues, heightening susceptibility to allergic reactions. Thus, the polluted atmosphere of a city doesn’t just introduce potential allergens; it also fundamentally alters the body's defensive systems, making the population more prone to developing sinus allergies.
Altered Living Environments
The shift in living environments within urban areas also impacts sinus allergy rates. Modern urban dwellings are frequently built with materials that foster mold growth, particularly in damp environments. Moreover, the prevalence of central heating and air conditioning systems, while offering comfort, can also spread allergens like dust mites and mold spores throughout homes and offices. Changes to lifestyle, such as the increasing amount of time spent indoors, can worsen the effect. Reduced natural ventilation limits the dispersal of indoor allergens. In essence, the indoor environments of cities can act as breeding grounds for allergens, leading to prolonged exposure and triggering allergic reactions. Consequently, the combination of building materials, HVAC systems, and lifestyle choices creates a setting highly favorable to the development and persistence of sinus allergies.
Immune System Adaptations
Urban lifestyles can also influence the way our immune systems operate, with implications for sinus allergies. The 'hygiene hypothesis' suggests that a lack of early-life exposure to diverse microbes in a cleaner urban environment may lead to a weaker immune system. This could mean the immune system becomes more likely to overreact to harmless substances, like pollen or dust mites. Besides, the higher stress levels often associated with urban life can further suppress immune function or alter the way the immune system responds to allergens. Chronic stress is known to increase inflammation, exacerbating allergic symptoms. This combination of an altered microbial environment, and stress-related immune changes helps set the stage for the body to develop increased sensitivity to allergens. As a result, the immune system in an urban context may become sensitized to environmental triggers, thus increasing the chance of allergic rhinitis.
Dietary and Lifestyle Effects
Dietary habits and lifestyle choices also influence the prevalence of sinus allergies, especially in urban environments. The modern urban diet, frequently processed and less diverse, can affect the body's inflammatory response. Some studies suggest a diet low in fruits, vegetables, and antioxidants may lead to an imbalance in the immune system, making it more prone to overreacting to allergens. Furthermore, urban lifestyles often involve less physical activity and more exposure to stress. Exercise is known to have anti-inflammatory effects, while chronic stress can amplify inflammation, which worsens allergic responses. Exposure to various chemicals and toxins in the environment can also impact immune function and allergic reactions. As a result, the combination of urban dietary patterns, activity levels, and stress levels creates a complex web of interactions that could potentially worsen or create the conditions for sinus allergies.
Mitigating Allergen Exposure
Reducing the impact of sinus allergies in urban environments involves multiple strategies, starting with limiting allergen exposure. Using air purifiers with HEPA filters inside the home and at work can significantly reduce exposure to indoor allergens like dust mites and mold spores. Keeping windows closed during high-pollen seasons also minimizes outdoor allergen entry. Regular cleaning, including vacuuming and dusting, is essential to remove allergens. For outdoor environments, wearing masks in polluted areas can limit the inhalation of irritants. Furthermore, consider showering and changing clothes after spending time outside. By implementing these practices, individuals can decrease their daily exposure to airborne allergens and reduce the severity of their sinus allergy symptoms.
Seeking Medical Assistance
When dealing with sinus allergies, seeking professional medical assistance is often crucial for effective management. If over-the-counter medications fail to provide adequate relief, consulting with a doctor or an ENT (Ear, Nose, and Throat) specialist becomes important. A healthcare professional can perform allergy tests to identify the specific allergens triggering the reaction, allowing for more targeted treatment. Treatment may involve prescription medications like antihistamines, nasal corticosteroids, or decongestants. In certain instances, immunotherapy, or allergy shots, might be recommended to desensitize the body to specific allergens over time. Additionally, an ENT can assess if the allergy has led to complications such as sinus infections and provide suitable treatment. Early and proper medical intervention can enhance quality of life, prevent the progression of severe symptoms and potential chronic complications.