What is Celiac Disease?
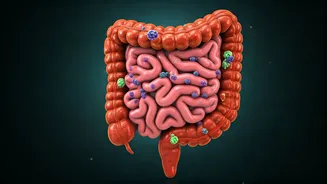
Celiac disease is a serious genetic autoimmune disorder where ingesting gluten, a protein found in wheat, barley, and rye, triggers an immune response
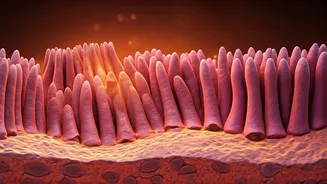
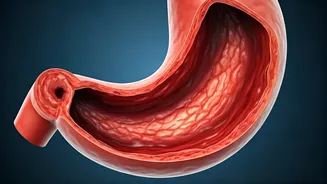
that attacks and damages the small intestine. This condition affects approximately 1 in 100 individuals globally, yet a significant portion, about 70%, remain undiagnosed. The immune system's overreaction to gluten leads to the erosion of villi, the finger-like projections within the small intestine responsible for nutrient absorption. This damage impairs the body's ability to absorb essential nutrients, leading to various health issues. While some symptoms may mimic gluten intolerance, celiac disease involves direct damage to the intestinal lining, a key differentiator from non-celiac gluten sensitivity.
The Genetic Link
The predisposition to celiac disease is strongly linked to an individual's genetic makeup. If you have a first-degree relative, such as a parent or sibling, who has been diagnosed with celiac disease, your risk factor of developing the condition increases to approximately 1 in 10. This genetic component means that certain individuals are inherently more susceptible to the autoimmune reaction triggered by gluten. While genetics are a crucial factor, they are not the sole determinant. Environmental factors, particularly gluten exposure, are necessary for the disease to manifest. Understanding this genetic link is vital for early detection and management, especially within families with a history of the condition.
Celiac vs. Gluten Intolerance
It's important to distinguish celiac disease from gluten intolerance, also known as non-celiac gluten sensitivity. While both conditions can cause digestive discomfort and other symptoms upon consuming gluten, the underlying mechanisms are different. In celiac disease, the immune system erroneously targets the small intestine, causing damage to the villi. This damage directly impacts nutrient absorption. Conversely, individuals with gluten intolerance may experience unpleasant symptoms like bloating, gas, or abdominal pain after eating gluten, but their small intestine remains structurally unimpaired. There is no autoimmune attack or damage to the villi in gluten intolerance. Therefore, while symptoms might overlap, the medical implications and diagnostic approaches for celiac disease and gluten intolerance are distinct.