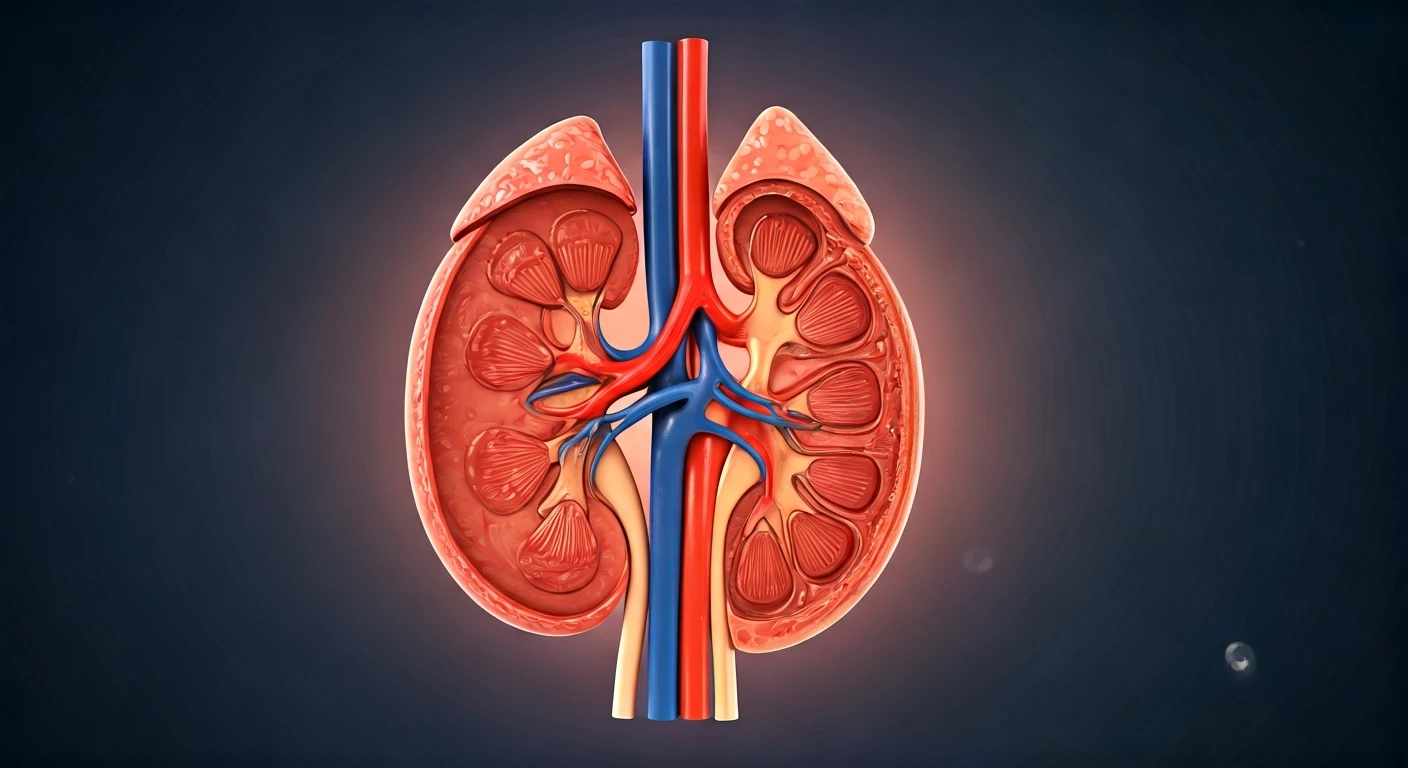
Understanding Kidney Disease Stages
Chronic Kidney Disease (CKD) progresses through five distinct stages, each characterized by decreasing kidney function. Stage 2 is considered mild, often
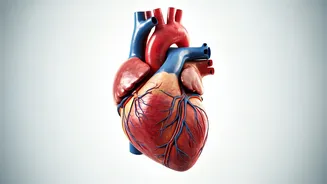
presenting no noticeable symptoms, making early detection crucial. Stage 3 signifies more significant kidney damage, and while not curable, proactive management can help halt its advancement and reduce the risk of complications. As the disease progresses to Stage 4, kidney damage becomes severe and irreversible. The most critical phase is End-Stage Kidney Disease (ESRD), where the kidneys have largely ceased to function, necessitating immediate and intensive treatment. Recognizing the signs of worsening kidney disease is vital; this includes monitoring specific symptoms and sharing this information with healthcare providers to tailor treatment plans effectively. Managing CKD also involves protecting cardiovascular health, especially for individuals with co-existing conditions like diabetes. Heart health tips are paramount for those with diabetes and kidney disease, focusing on lifestyle adjustments that benefit both conditions simultaneously.
Complications and Advanced Stages
As kidney disease advances, it can lead to a range of complications that significantly impact quality of life. One common and distressing symptom in later stages is chronic itching, a condition that requires specific management strategies to alleviate discomfort. The overall impact of CKD on kidney function can manifest in various ways, affecting the entire body. For individuals with ESRD, the kidneys have failed to the point where external intervention is essential for survival. Understanding the severe, irreversible damage of Stage 4 kidney disease is crucial for patients and their families to prepare for the necessary treatment pathways. This stage often marks a significant shift in medical care and requires close monitoring by healthcare professionals to manage symptoms and prevent further deterioration.
Navigating Dialysis Treatments
Dialysis is a critical life-sustaining treatment for individuals with end-stage kidney disease, involving a machine to filter and purify the blood. Understanding the different types of dialysis, such as hemodialysis and peritoneal dialysis, is essential for making informed decisions. Hemodialysis, the more common method, uses an artificial kidney to clean the blood, while peritoneal dialysis utilizes the lining of the abdomen as a filter. Both procedures have their own set of benefits and potential risks that patients must weigh. It's also important to be aware of the possible side effects associated with dialysis and to discuss strategies with healthcare providers to manage them effectively, aiming to improve comfort and well-being during treatment. Furthermore, understanding how dialysis is covered by insurance, specifically Medicare for End-Stage Renal Disease (ESRD), is vital for financial planning and ensuring access to necessary care. This coverage often includes eligibility criteria and details on what aspects of treatment are supported.
Alternative and Supportive Care
Beyond dialysis, various treatment options exist for kidney failure. A kidney transplant offers a more definitive solution by replacing the damaged kidneys with a healthy donor organ, presenting high success rates and often being the preferred treatment for eligible candidates. Medical management also focuses on maintaining existing kidney function and managing symptoms without solely relying on dialysis. This approach aims to preserve what remains of the kidneys' capabilities. Patient experiences can vary widely, and perspectives from individuals within specific communities, such as the BIPOC community, highlight unique challenges and journeys in accessing care for chronic kidney disease. Advocacy and shared experiences play a significant role in improving care pathways. Finding support is also paramount; this includes connecting with others who have CKD through support groups, accessing financial assistance programs, and understanding the mental health impact of the disease.
Diet, Lifestyle, and Well-being
Managing chronic kidney disease extends beyond medical treatments to encompass crucial dietary and lifestyle modifications. Fatigue is a pervasive symptom for many with CKD, and strategies like consistent sleep and regular exercise can help mitigate its effects. Nutritional intake, particularly protein, requires careful consideration; consuming too much protein can strain compromised kidneys, thus a controlled intake is often recommended. Kidney disease can also contribute to weight gain due to the body retaining excess water, necessitating mindful fluid and sodium management. Specific dietary restrictions are common, with a list of around 17 foods often advised to be avoided due to their high potassium, phosphorus, or sodium content. Furthermore, the link between diabetes, depression, and kidney disease is significant; managing both diabetes and depression is vital to prevent the onset or worsening of kidney issues. Mental well-being is central to managing CKD, as the condition can impact mental health, leading to increased risks of stress, anxiety, and depression. Resources and support systems are available to help individuals navigate these challenges.