Antibiotics and Gut Health
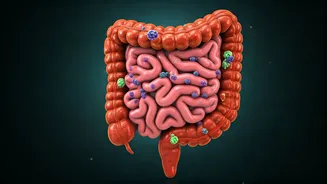
Antibiotics, designed to fight bacterial infections, can unfortunately impact the intricate ecosystem within your gut. They don't just target the bad bacteria;
they also wipe out the beneficial ones. This indiscriminate action can lead to a shift in the gut's microbial balance, known as dysbiosis. This disruption paves the way for various health problems. Recognizing the delicate relationship between antibiotics and gut health is the first step toward understanding the potential risks and adopting proactive strategies for maintaining optimal digestive well-being. It is important to note that antibiotics may be necessary in several cases, and this article aims to help create awareness of the side effects of their excessive usage.
Diarrhea as a Result
Diarrhea is a very common and immediate side effect of antibiotic use. Antibiotics, particularly broad-spectrum ones, upset the natural balance of bacteria in the gut, disrupting the digestive process and leading to loose, watery stools. The severity of the diarrhea varies depending on the antibiotic type, dosage, and the individual's gut microbiome composition. In some instances, it may be mild and temporary, while in others, it can be persistent and debilitating. To prevent diarrhea, one should always use antibiotics only when prescribed by a doctor, and, if it occurs, one should consider taking probiotics to help restore the gut flora.
Risk of C. difficile
One of the most concerning complications associated with antibiotic use is the increased risk of developing Clostridioides difficile (C. diff) infection. Antibiotics disrupt the normal gut flora, creating an environment where C. diff, a bacterium resistant to many antibiotics, can flourish. This can result in severe diarrhea, abdominal pain, and, in some cases, life-threatening inflammation of the colon (colitis). C. diff infections can be difficult to treat and often require specific antibiotics or even fecal microbiota transplantation to restore a healthy gut environment. Preventing this infection involves prudent antibiotic use and possibly probiotic supplementation under medical guidance.
Nausea and Vomiting
Besides diarrhea, nausea and vomiting can also occur with the use of antibiotics. These are often related to the disruption of gut flora, which can affect the way your gut functions. The imbalance in the gut microbiome may trigger inflammation and irritation of the gastrointestinal tract, leading to these uncomfortable symptoms. The specific antibiotic type, its dosage, and an individual's sensitivity influence how severe these symptoms will be. Taking antibiotics with food or ensuring adequate hydration can sometimes help mitigate nausea and vomiting. If the symptoms are severe or persistent, it's essential to consult a healthcare provider for possible solutions or a change in medication.
Abdominal Pain/Cramps
Antibiotics can cause abdominal pain and cramping. The disturbances in the gut's normal bacterial balance may lead to inflammation, gas build-up, and altered bowel movements, all contributing to discomfort. The pain may range from mild, intermittent cramps to severe, persistent abdominal pain. Some antibiotics are more likely to cause these symptoms than others. Taking antibiotics with food can sometimes help to alleviate abdominal discomfort. If the pain is severe or accompanied by other symptoms like fever or bloody stools, it is essential to seek medical advice.
Impact on Nutrient Absorption
The gut microbiome plays a crucial role in nutrient absorption, and antibiotics can hinder this process. The imbalance of gut bacteria reduces the body's capacity to absorb nutrients from food, potentially leading to deficiencies of essential vitamins and minerals. The extent of this effect varies depending on the specific antibiotic, duration of use, and an individual's gut composition. The prolonged malabsorption can result in fatigue, weakness, and other health issues. Supporting gut health through a balanced diet, probiotic use, and the judicious use of antibiotics can help maintain optimal nutrient absorption.
Yeast Infections Rise
Antibiotics may increase the risk of yeast infections, especially in women. The depletion of gut bacteria can disrupt the natural balance, fostering the overgrowth of yeast, particularly Candida albicans. This overgrowth can lead to vaginal yeast infections and oral thrush. The use of certain antibiotics and the individual's susceptibility influence the risk of yeast infections. Taking probiotics and maintaining good hygiene practices may help mitigate this risk. If yeast infections do occur, over-the-counter or prescription antifungal medications may be needed.
Weight Gain Risks
Surprisingly, antibiotics can also contribute to weight gain, although the mechanism is complex. Changes in the gut microbiome can influence metabolism and energy storage, increasing the risk of weight gain in some people. Alterations in gut bacteria can affect how the body processes food, leading to increased fat storage and changes in appetite. Specific antibiotics and the individual's gut composition play a role in this. Maintaining a balanced diet, regular exercise, and possibly probiotic use can help mitigate the risk of antibiotic-related weight gain. It is advisable to consult a healthcare provider for personalized advice.
Altered Gut Microbiome
The long-term effects of antibiotics on the gut microbiome can be profound. Antibiotics may reduce the diversity of gut bacteria, and it can take months or even years for the gut ecosystem to fully recover after antibiotic use. The alterations in the gut microbiome may affect immune function, digestion, and overall health. The specific antibiotic, the duration of use, and the individual's gut composition influence the extent of these changes. Supporting gut health through diet, probiotics, and, when possible, minimizing unnecessary antibiotic use is essential to help restore and maintain a balanced gut microbiome.
Antibiotic Resistance Concerns
One of the most significant long-term concerns is the development of antibiotic resistance. Frequent antibiotic use contributes to the rise of antibiotic-resistant bacteria, making infections harder to treat in the future. Bacteria can adapt and evolve, becoming less susceptible to antibiotics. Prudent use of antibiotics, only when necessary and prescribed by a healthcare professional, can help prevent antibiotic resistance. Taking appropriate measures to prevent infections, such as good hygiene practices and vaccination, also plays a crucial role in reducing the need for antibiotics and therefore, their long-term health risks.