Early Stages Explained
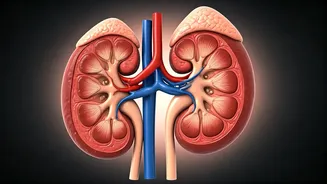
Chronic Kidney Disease (CKD) often progresses silently in its initial phases. Stage 2 CKD, considered mild, may present no noticeable symptoms, making
early detection challenging but crucial. Similarly, Stage 3 CKD, while still manageable with early diagnosis to potentially halt further deterioration and reduce associated health risks, requires vigilance. Recognizing the signs that your kidney disease might be worsening is paramount. These indicators could include subtle changes in how you feel or appear, prompting a need to meticulously track symptoms. This proactive approach allows for informed discussions with healthcare providers, ensuring timely interventions. Furthermore, for individuals managing both diabetes and kidney disease, protecting heart health becomes a critical focus, with specific strategies available to mitigate cardiovascular risks inherent in this dual diagnosis. Understanding these early markers empowers patients to take control of their health trajectory from the outset.
Advanced CKD and Complications
As Chronic Kidney Disease (CKD) advances, its impact becomes more profound and potentially irreversible. Stage 4 CKD signifies severe kidney damage, where function is significantly compromised. The ultimate progression is End-Stage Kidney Disease (ESKD), also known as end-stage renal disease (ESRD), a state where the kidneys have nearly or completely ceased to function. This severe decline can lead to a cascade of complications affecting various bodily systems. One particularly distressing symptom that often emerges in advanced CKD is persistent itching, which can significantly impact a patient's comfort and well-being. Managing these advanced stages requires a comprehensive understanding of the potential complications and proactive strategies to alleviate symptoms and maintain the best possible quality of life.
Navigating Dialysis and Alternatives
When kidneys reach end-stage renal disease (ESRD), dialysis becomes a critical life-sustaining treatment, acting as an artificial filter to purify the blood. Understanding the various types of dialysis, such as hemodialysis and peritoneal dialysis, is essential for patients and their families. Hemodialysis typically involves using a machine to cleanse the blood externally, while peritoneal dialysis uses the body's own lining to filter waste. Both methods have distinct procedures, benefits, and potential risks that require careful consideration. Beyond the mechanics of dialysis, it's vital to be aware of possible side effects, which can range from fatigue to more specific discomforts, and to learn management strategies. For many, the question of financial coverage arises, and understanding options like Medicare coverage for ESRD is crucial. While dialysis is a primary treatment, exploring alternatives like kidney transplantation, which offers a more permanent solution, and other medical management strategies that focus on preserving existing kidney function, provides a broader perspective on managing kidney failure.
Holistic Management: Diet and Well-being
Living with Chronic Kidney Disease (CKD) extends beyond medical treatments to encompass significant lifestyle and dietary adjustments. Managing fatigue, a common challenge for CKD patients, can be addressed through adequate sleep and regular, appropriate exercise. Dietary choices are paramount; for instance, understanding the precise protein intake needed is vital, as consuming too much can strain compromised kidneys. Furthermore, CKD can affect fluid balance, leading to unexpected weight gain, which necessitates careful monitoring. Specific food restrictions are also common, with guidance often suggesting avoiding certain items high in potassium, phosphorus, and sodium to protect remaining kidney function. Beyond the physical, CKD can profoundly impact mental health, increasing the risk of stress, anxiety, and depression. Accessing support networks, whether through patient advocacy, support groups, or financial assistance programs, is integral to navigating the emotional and practical challenges of living with CKD, fostering resilience and a better overall outlook.