Understanding Diabetes Remission
Diabetes remission signifies a significant shift in managing Type 2 diabetes, where blood sugar levels return to a normal range without medication. However,
it's vital to clarify that remission doesn't equate to a cure. It's a state where the disease is under control, and the need for diabetes medications may be reduced or eliminated. Remission can be achieved through various methods, encompassing lifestyle modifications like diet changes and increased physical activity, as well as medical interventions. The specific approach depends on individual factors and the guidance of healthcare professionals. It's crucial to consult a doctor to determine the best course of action and continuously monitor health indicators.
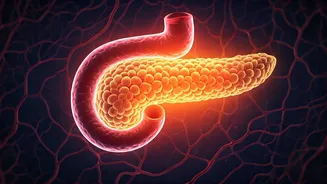
The Science Behind Reversal
Recent research reveals that weight loss, particularly through dietary interventions and exercise, plays a crucial role in diabetes remission. Studies highlight the impact of reducing fat in the liver and pancreas, which can improve insulin sensitivity and restore the function of insulin-producing cells. These findings underscore the importance of lifestyle modifications. The scientific community continues to explore the mechanisms of remission, which contributes to developing effective strategies.
Dietary Strategies Explained
Dietary changes form a foundational element in achieving diabetes remission. A diet low in processed foods, refined carbohydrates, and sugary drinks is often recommended. This approach supports blood sugar control and encourages weight loss. Incorporating a balance of whole foods, lean proteins, and healthy fats is crucial. Consulting a registered dietitian can create a personalized meal plan, tailored to your unique needs and preferences. This guidance is important to the creation of a sustainable, long-term approach to eating.
The Role of Exercise
Regular physical activity is another critical aspect of diabetes management and remission. Exercise improves insulin sensitivity, assists in weight loss, and enhances cardiovascular health. A combination of aerobic exercises (like brisk walking) and resistance training (such as weightlifting) is often recommended. It’s important to select activities that you find enjoyable. Start gradually, and progressively increase the intensity and duration of your workouts. Before starting a new exercise regimen, consult your doctor. They can give tailored guidance based on your health status.
Medical Interventions and Support
In addition to lifestyle changes, medical interventions may be considered. These could include medication adjustments or, in some instances, bariatric surgery. Working with a multidisciplinary team—doctors, dietitians, and certified diabetes educators—ensures a comprehensive approach. Regular monitoring of blood sugar levels, along with periodic check-ups, is essential. This also ensures that any adjustments can be made as needed, so you can achieve the best possible outcomes.
Maintaining Long-Term Health
Sustaining remission requires a long-term commitment to healthy habits. This includes consistently following dietary recommendations, staying active, and attending regular medical check-ups. Moreover, being aware of and managing stress is essential for overall well-being. Developing a support network of friends, family, or support groups offers encouragement and helps maintain motivation. This strategy is essential for achieving a healthier and more fulfilling life.