Early Testing Matters
The decision on when to get a cholesterol test is a significant one. The general consensus emphasizes the importance of early testing, as it allows for
the early detection of potential health risks. Early identification can lead to timely interventions, such as lifestyle adjustments and, when required, medical treatments. These steps can significantly reduce the risks associated with elevated cholesterol levels, protecting long-term health. Knowing your cholesterol levels at a young age provides a baseline to monitor changes over time. This approach allows doctors to track trends and make personalized recommendations based on your unique health profile. Starting early is all about preventative healthcare, empowering individuals to take control of their cardiovascular health before problems develop.
Risk Factors Explained
Several risk factors help determine the ideal time to get a cholesterol test. These include family history, lifestyle choices, and existing health conditions. A strong family history of heart disease or high cholesterol should prompt earlier and more frequent testing. Unhealthy habits such as a poor diet high in saturated and trans fats, lack of exercise, and smoking, can increase your risk. Conditions like diabetes, high blood pressure, and obesity also increase the likelihood of elevated cholesterol levels, making early testing a necessity. Your doctor will weigh these factors to create a testing schedule that is tailored to your individual risk profile. Early and proactive monitoring, especially when risk factors are present, is crucial for maintaining heart health and mitigating potential future issues.
Testing Guidelines Overview
Understanding testing guidelines will help you schedule your cholesterol check. Guidelines often suggest that adults without risk factors should start screening at age 20 and repeat testing every 4 to 6 years. For those with risk factors, more frequent testing may be required, potentially beginning even earlier in life. Your doctor will make a specific recommendation based on an assessment of your personal risk profile and overall health. The frequency of tests may also depend on your cholesterol levels and any treatment you are receiving. Following established guidelines helps ensure that you receive timely care and maintain cardiovascular health. If you are uncertain about when to begin, consulting a healthcare professional is always the best approach.
Interpreting Test Results
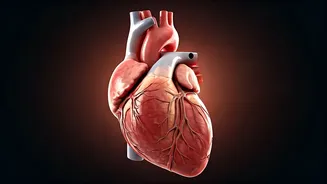
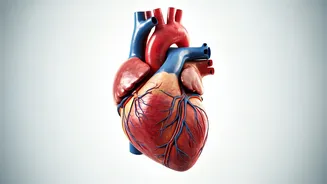
Understanding how to interpret your cholesterol test results is also important. The test typically measures several types of lipids, including total cholesterol, LDL (low-density lipoprotein or 'bad' cholesterol), HDL (high-density lipoprotein or 'good' cholesterol), and triglycerides. Desirable levels for LDL cholesterol typically should be below 100 mg/dL, while the higher the HDL, the better. Your doctor will help you interpret your results, explaining any levels that are outside the normal range. Elevated LDL cholesterol is a primary concern, as it can contribute to the buildup of plaque in arteries. HDL cholesterol helps remove cholesterol from the arteries, reducing risk. Triglycerides, also measured in the test, are another type of fat in the blood, and elevated levels also increase the risk of heart disease. Consulting with your healthcare provider will give you a clear understanding of your results and what steps you may need to take to maintain optimal heart health.
Lifestyle Adjustments
Lifestyle changes can significantly influence your cholesterol levels, and understanding how to implement these changes is beneficial. Diet plays a crucial role in managing cholesterol. Limiting saturated and trans fats, found in processed foods and some animal products, can help lower LDL cholesterol. Incorporating foods rich in soluble fiber, such as oats, beans, and fruits, can also help. Regular physical activity has been shown to improve HDL cholesterol and help lower LDL. Aim for at least 150 minutes of moderate-intensity exercise per week. Quitting smoking will also raise your HDL and improve overall cardiovascular health. Making these adjustments can positively affect your cholesterol levels, improving overall health and minimizing your risk of heart-related issues. Your doctor can offer personalized advice and resources to assist you in making these changes effectively.
Medical Treatments Options
When lifestyle changes alone are insufficient to manage high cholesterol, medical treatments may be necessary. Statins are a common type of medication that helps lower LDL cholesterol by reducing its production in the liver. Other medications, like fibrates, can help lower triglycerides, and bile acid sequestrants work by preventing the absorption of cholesterol in the intestines. Your doctor will prescribe the most appropriate medication based on your cholesterol levels, overall health, and any existing medical conditions. It’s also important to remember that these medications should be taken as prescribed. Regular follow-up appointments with your doctor are crucial to monitor their effectiveness and manage potential side effects. Pairing medications with lifestyle changes is the most comprehensive strategy for effectively managing high cholesterol and reducing the risk of heart-related issues.