Calcium's Vital Functions
Calcium is a mineral that plays an essential part in many biological processes. It is a fundamental component of bones and teeth, providing them with structure
and strength. Furthermore, it is critical for nerve impulse transmission, muscle contraction, and blood clotting. Calcium ions are involved in the electrical activity of the heart, allowing it to beat regularly. The regulation of calcium levels is tightly controlled by the body through hormones like parathyroid hormone and vitamin D, ensuring that adequate amounts are available for these vital functions. It is, therefore, clear how important this mineral is to maintain basic body functions.
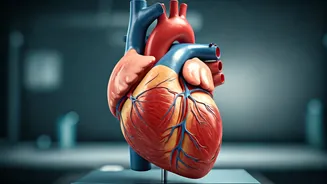
Cardiac Calcification Defined
Cardiac calcification is a condition characterized by the deposition of calcium in the heart. This accumulation can happen in several areas, including the coronary arteries, heart valves, and the heart muscle itself. The process often develops gradually over time, frequently associated with the aging process and other health conditions. This build-up of calcium can lead to various cardiovascular problems, making it a significant concern for heart health. The underlying mechanisms, which often involve inflammation, oxidative stress, and lipid accumulation, lead to this accumulation. Recognizing and addressing cardiac calcification is vital for preserving heart function.
Factors Behind Accumulation
Several factors contribute to the buildup of calcium in the heart. One major risk is atherosclerosis, where the arteries become hardened and narrowed due to plaque buildup. This plaque often contains calcium deposits. Other conditions like chronic kidney disease can disrupt calcium-phosphate balance, leading to vascular calcification. Inflammation and oxidative stress also play a crucial role in promoting calcification. Certain lifestyle choices, such as a poor diet high in saturated fats and a lack of exercise, can increase the risk. Additionally, genetic predispositions can influence the likelihood of developing cardiac calcification. Understanding the interplay of these various factors is essential for managing the risk.
Health Implications Explained
The accumulation of calcium in the heart poses several significant health risks. Calcification in the coronary arteries can narrow the arteries, leading to reduced blood flow and potentially causing angina (chest pain) or even heart attacks. If the heart valves become calcified, this can disrupt their function, making it harder for the heart to pump blood efficiently. This can result in heart failure. Furthermore, cardiac calcification can lead to arrhythmias (irregular heartbeats), increasing the risk of sudden cardiac arrest. The severity of these health issues depends on the amount and location of the calcium buildup, underscoring the importance of early detection and management.
Diagnosis and Detection
Detecting cardiac calcification often involves imaging tests. Coronary artery calcium (CAC) scoring using computed tomography (CT) scans is a common method for assessing the amount of calcium in the coronary arteries. Other diagnostic tools include echocardiograms, which visualize heart valves and the heart muscle, and cardiac catheterization, which is a more invasive procedure, also used to visualize arteries and valves. Regular checkups and screenings, especially for individuals with risk factors, are essential for early detection. The information gained from these diagnostic procedures helps in formulating effective treatment strategies and monitoring disease progression. Early detection ensures timely intervention.
Preventative Measures Explored
Preventing cardiac calcification involves making lifestyle changes and managing underlying health conditions. A heart-healthy diet low in saturated and trans fats and high in fruits, vegetables, and whole grains is important. Regular exercise is also crucial for maintaining cardiovascular health. Managing conditions like high blood pressure, high cholesterol, and diabetes is essential, as these conditions increase the risk of calcium buildup. Avoiding smoking and limiting alcohol consumption are other preventative measures. Regular health checkups, including monitoring blood pressure, cholesterol levels, and kidney function, can help detect problems early, which can allow intervention and improve outcomes.
Treatment Options Outlined
Treating cardiac calcification depends on the severity of the condition and the symptoms presented. For mild cases, lifestyle modifications and medication to control risk factors may be sufficient. More severe cases might require medical interventions. In the event of narrowed arteries, angioplasty and stenting may be used to open them. Valve replacement surgery is necessary if the valves are severely damaged. Medications, such as statins to lower cholesterol, blood pressure medications, and blood thinners, may be prescribed. The treatment plan is always individualized, and regular monitoring by a healthcare professional is crucial to manage and slow the progression of the disease.