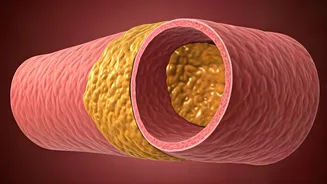
Plaque: The Culprit
Plaques within arteries, are the primary concern when considering heart health. These plaques are made up of cholesterol, fatty substances, cellular waste,
calcium, and fibrin. Initially, these plaques may not cause noticeable symptoms, often going unnoticed for quite some time. Over time, these plaques can grow and harden, narrowing the arteries and reducing blood flow. This reduced blood flow can cause various problems, including chest pain (angina), shortness of breath, and an increased risk of heart attack or stroke. Understanding how these plaques form and what contributes to their growth is the first step toward promoting better cardiovascular health and taking proactive measures.
Formation Explained
The formation of arterial plaques is a complex process. It generally starts with damage to the inner lining of the artery, known as the endothelium. This damage can be caused by various factors, including high blood pressure, smoking, high cholesterol, high blood sugar, and chronic inflammation. When the endothelium is damaged, it becomes more permeable, allowing LDL cholesterol (often called "bad" cholesterol) to penetrate the artery wall. The LDL cholesterol then becomes oxidized and triggers an inflammatory response. The immune system sends macrophages to the site, which engulf the oxidized LDL cholesterol and become foam cells. Over time, these foam cells accumulate, forming a fatty streak, which is the precursor to a plaque. The plaque continues to grow as more cholesterol, immune cells, and fibrous tissue are deposited.
Reversing the Damage
While it can be challenging, there are strategies to potentially reverse arterial plaque buildup and improve heart health. The approach mainly focuses on lifestyle modifications and, in some cases, medical interventions. Dietary changes are critical. This involves adopting a heart-healthy diet low in saturated and trans fats, cholesterol, and added sugars, and rich in fruits, vegetables, whole grains, and lean proteins. Regular physical exercise is also very beneficial. Exercise helps lower LDL cholesterol, raise HDL cholesterol (the "good" cholesterol), and improve overall cardiovascular function. Quitting smoking is paramount, as smoking significantly damages the arteries. Managing stress through techniques like meditation and yoga can also contribute to heart health. Furthermore, prescribed medications can help manage cholesterol levels, blood pressure, and other risk factors.
Dietary Interventions
A heart-healthy diet forms the bedrock of strategies to combat arterial plaque. This diet should emphasize the consumption of whole, unprocessed foods. Fruits and vegetables are rich in antioxidants and fiber, which protect against oxidative damage and help lower cholesterol levels. Whole grains, such as oats, brown rice, and quinoa, offer fiber, which can help reduce LDL cholesterol. Lean proteins, including fish rich in omega-3 fatty acids, poultry without skin, and plant-based protein sources like beans and lentils, should be preferred over red and processed meats. Limiting saturated and trans fats found in processed foods, fried foods, and some animal products, as well as minimizing added sugars, is crucial. Additionally, incorporating healthy fats such as those found in avocados, nuts, and olive oil can provide benefits. Consistent dietary adjustments can significantly improve arterial health and reduce the risk of plaque-related complications.
The Role of Exercise
Regular physical activity plays a pivotal role in maintaining and improving heart health, specifically in managing the effects of arterial plaque. Exercise helps improve the ratio of HDL (good) cholesterol to LDL (bad) cholesterol. Activities like brisk walking, jogging, swimming, or cycling are highly effective for cardiovascular health. Aim for at least 150 minutes of moderate-intensity exercise per week, or 75 minutes of vigorous-intensity exercise. In addition to improving cholesterol levels, exercise also helps lower blood pressure, improve insulin sensitivity, and reduce inflammation, all of which are significant factors in plaque formation and progression. Incorporating both aerobic and resistance training provides comprehensive benefits. Consistent physical activity is a crucial element in a multifaceted strategy to reverse and prevent arterial plaque formation.
Other Lifestyle Changes
Beyond diet and exercise, other lifestyle changes significantly impact arterial health. The most critical step is to quit smoking, as smoking severely damages the arteries and accelerates plaque formation. Managing stress through techniques like meditation, yoga, or other relaxation methods is also vital. Chronic stress can contribute to inflammation and elevated blood pressure, further promoting plaque buildup. Adequate sleep, typically 7-8 hours per night, supports overall health and cardiovascular well-being. Excessive alcohol consumption should also be avoided, as it can raise blood pressure and contribute to heart disease. Regular health check-ups and monitoring of cholesterol levels, blood pressure, and blood sugar are essential for early detection and intervention. Making these lifestyle adjustments will enhance your efforts to combat arterial plaque and improve heart health.
Medical Interventions
In addition to lifestyle modifications, medical interventions can be necessary to manage and reverse arterial plaque, depending on the severity and progression of the condition. Statins are a frequently prescribed medication that helps lower LDL cholesterol levels. Other medications, such as fibrates and niacin, may also be used to manage cholesterol. Blood pressure medications, including ACE inhibitors, ARBs, and beta-blockers, are often prescribed to control high blood pressure, which contributes to plaque formation. In some cases, when arteries become severely blocked, procedures like angioplasty or coronary artery bypass surgery may be necessary to restore blood flow. Angioplasty involves inserting a catheter with a balloon to widen the artery, while bypass surgery creates a new pathway for blood flow around the blocked artery. The choice of medical interventions depends on individual circumstances and the advice of a healthcare professional.