What is Psoriasis?
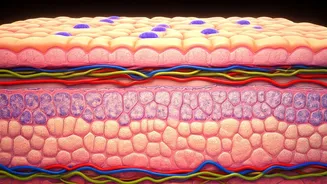
Psoriasis is a chronic autoimmune condition that primarily affects the skin, causing rapid skin cell growth. The usual skin cell life cycle is about a month,
but in psoriasis, this cycle speeds up, leading to a build-up of cells on the skin's surface. These excess skin cells form thick, scaly patches that can be itchy, painful, and often unsightly. The condition can manifest in various forms, impacting different areas of the body and varying in severity. While the exact causes are not fully understood, it is believed to be a combination of genetic factors and environmental triggers. Certain triggers, such as stress, skin injuries, infections, and specific medications, can worsen the condition. People with psoriasis also experience an increased risk of other health issues, including psoriatic arthritis, a form of arthritis that affects the joints.
Types of Psoriasis
Psoriasis presents in several distinct types, each characterized by unique symptoms and affected areas of the body. Plaque psoriasis is the most common form, causing raised, red patches covered with silvery scales, often found on the elbows, knees, scalp, and lower back. Guttate psoriasis typically appears as small, drop-shaped lesions on the trunk, arms, and legs, often triggered by a bacterial infection. Inverse psoriasis manifests in skin folds, such as the armpits, groin, and under the breasts, causing smooth, red patches. Pustular psoriasis is characterized by pus-filled blisters surrounded by red skin, and can affect large areas of the body. Erythrodermic psoriasis is a severe and rare form causing widespread redness, scaling, and shedding of the skin, sometimes requiring hospitalization. Identifying the specific type is important for effective treatment strategies.
Identifying Triggers
Several factors can trigger or worsen psoriasis symptoms. Stress is a significant contributor, with both emotional and physical stress linked to flare-ups. Skin injuries, such as cuts, scrapes, insect bites, or sunburns, can provoke the condition in a phenomenon known as the Koebner phenomenon. Infections, particularly those caused by bacteria like streptococcus, can also act as triggers. Certain medications, including lithium, beta-blockers, and antimalarial drugs, may exacerbate psoriasis. Climate can play a role; cold, dry weather may worsen symptoms, while sunlight can sometimes improve them. Understanding personal triggers is key to managing psoriasis. Maintaining a journal to track potential triggers, and consulting a healthcare professional can assist in identifying and minimizing flare-ups, and formulating a proactive management plan that incorporates lifestyle adjustments and medical treatments.
Treatment Strategies Explored
Managing psoriasis involves a multi-faceted approach, incorporating both lifestyle changes and medical treatments to alleviate symptoms. Topical treatments, such as corticosteroids, vitamin D analogs, and retinoids, are often the first line of defense, reducing inflammation and slowing skin cell growth. Phototherapy, or light therapy, using ultraviolet (UV) light, can also be beneficial in reducing inflammation. For more severe cases, systemic medications, including methotrexate, cyclosporine, and biologics, may be prescribed. Biologics, which target specific parts of the immune system, have shown great effectiveness, but may have potential side effects. Lifestyle adjustments are crucial, including maintaining a healthy diet, managing stress, and avoiding triggers. Regular moisturizing, proper skincare, and gentle cleansing can help alleviate symptoms and keep skin healthy. A dermatologist can offer personalized treatment recommendations to manage and control psoriasis effectively.
Living with Psoriasis
Living with psoriasis requires developing coping strategies to manage physical symptoms and emotional well-being. It is important to establish a consistent skincare routine. Regular moisturizing, using gentle soaps, and avoiding harsh scrubs are crucial to keeping the skin hydrated and healthy. Dietary adjustments, such as including anti-inflammatory foods, may help manage symptoms. Stress management techniques like yoga, meditation, or deep breathing can be highly beneficial. Joining support groups or connecting with others who have psoriasis can provide emotional support and practical advice. Open communication with healthcare providers and proactive participation in treatment plans are vital components in managing psoriasis effectively. By combining medical treatments with lifestyle modifications, individuals can improve their quality of life and effectively manage the challenges associated with the condition.