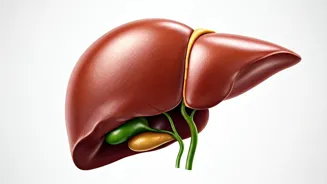
Understanding Fatty Liver
Fatty liver disease, a condition characterized by excessive fat accumulation in the liver, is becoming increasingly prevalent globally. The liver, vital
for detoxification and metabolism, can be significantly impaired by this buildup. There are two primary types: non-alcoholic fatty liver disease (NAFLD), not linked to excessive alcohol intake, and alcoholic fatty liver disease (AFLD), caused by heavy alcohol consumption. NAFLD is often associated with factors like obesity, diabetes, and high cholesterol. This article focuses on early indicators, understanding that early detection and intervention are critical. Recognizing early symptoms enables timely lifestyle changes, which can prevent the disease from progressing to more severe stages like cirrhosis or liver failure. Therefore, understanding the initial warning signs is crucial for anyone wanting to safeguard liver health and overall wellness. Recognizing these early indicators can lead to significant lifestyle adjustments, potentially halting or reversing the condition's progression. Early intervention significantly reduces the risk of severe complications.
Early Warning Signs
Several subtle signs may indicate a fatty liver, often appearing before more serious symptoms manifest. These early indicators are crucial for timely intervention. One common sign is fatigue and general weakness; persistent tiredness that doesn't improve with rest can indicate liver dysfunction. Another key sign is abdominal discomfort, particularly in the upper right quadrant, where the liver is located. This may manifest as a dull ache or a feeling of fullness. Other warning signs include unexplained weight loss, loss of appetite, and yellowing of the skin or eyes (jaundice), which indicates bilirubin buildup, which can signal liver issues. These signs are not exclusive to fatty liver, so a medical evaluation is necessary to confirm the diagnosis. Early detection allows for timely lifestyle changes, potentially preventing the disease from escalating to more severe stages, thus highlighting the importance of recognizing these signals and consulting with a healthcare professional for a comprehensive assessment.
Risk Factors Explained
Several factors increase the likelihood of developing fatty liver disease. Identifying and managing these factors is vital for prevention. Obesity, especially abdominal obesity, is a significant risk factor. Excessive body fat can lead to fat accumulation in the liver. Diabetes and insulin resistance also play a crucial role. People with diabetes often have impaired glucose metabolism, leading to fat buildup in the liver. High cholesterol and triglycerides, indicative of lipid imbalances, also increase the risk. An unhealthy diet high in processed foods, saturated fats, and sugary drinks exacerbates the issue. Excessive alcohol consumption, in the case of alcoholic fatty liver disease, is a direct cause. Genetics and family history may also play a role, with certain individuals being predisposed to the condition. Recognizing these risk factors enables you to proactively manage your health by adopting a healthy lifestyle, including a balanced diet, regular exercise, and, if necessary, medical management of related conditions such as diabetes and high cholesterol.
Dietary Changes for Health
Dietary adjustments play a crucial role in managing and potentially reversing fatty liver. The goal is to reduce the liver's workload and prevent further fat accumulation. A diet rich in fruits, vegetables, whole grains, and lean proteins is essential. Focus on foods with high fiber content, which help regulate blood sugar levels and promote liver health. Limiting processed foods, sugary drinks, and saturated fats is vital. Increase your intake of healthy fats, like those found in avocados, nuts, and olive oil. Include foods known to benefit the liver, such as coffee and green tea, which can help reduce inflammation. It is also important to stay hydrated by drinking plenty of water. Portion control is also critical, avoiding overeating and maintaining a healthy weight. Consider consulting a registered dietitian to create a personalized dietary plan that meets your needs and supports optimal liver function. Making these changes can significantly improve liver health and overall wellness.
Exercise and Activity
Regular physical activity is a cornerstone of managing fatty liver disease. Exercise promotes weight loss, improves insulin sensitivity, and reduces liver fat accumulation. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise each week. This could include activities like brisk walking, jogging, cycling, or swimming. Strength training exercises can also be beneficial, as they help build muscle mass and improve metabolism. It’s important to choose activities that you enjoy to ensure consistency. Even incorporating small amounts of activity throughout the day, such as taking the stairs instead of the elevator or going for short walks, can be beneficial. Regular physical activity also supports overall cardiovascular health and boosts energy levels, contributing to a better quality of life. Consistency is key. Making exercise a regular part of your routine, coupled with a healthy diet, significantly benefits your liver health and overall well-being.
Other Lifestyle Adjustments
Beyond diet and exercise, several lifestyle adjustments can improve liver health. Limiting or avoiding alcohol is crucial, especially for those with alcoholic fatty liver disease, and it is generally advisable for those with NAFLD. Maintaining a healthy weight is essential, as obesity significantly contributes to the disease. Managing existing health conditions, such as diabetes and high cholesterol, through medication and lifestyle changes is also crucial. Ensure sufficient sleep. Quality sleep supports the body's natural detoxification processes. Minimize exposure to toxins by avoiding unnecessary medications and environmental pollutants. Reduce stress through relaxation techniques like yoga, meditation, or deep breathing exercises. Consider consulting with healthcare professionals, including your doctor or a liver specialist, for personalized advice and regular checkups. These proactive changes can support liver health and prevent the progression of fatty liver disease, leading to improved overall well-being.