The Sleep-Insulin Link
The connection between sleep and metabolic health is increasingly recognized, with sleep playing a pivotal role in how our bodies process insulin. Insulin,
a hormone produced by the pancreas, is essential for regulating blood sugar levels. It allows glucose from the food we eat to enter our cells for energy. When sleep is disrupted, this delicate balance can be significantly thrown off. According to health experts, a single night of reduced sleep—specifically, sleeping only four hours—can lead to a surprising drop in insulin sensitivity. The impact is noteworthy, as a decrease in insulin sensitivity means our cells become less responsive to insulin. Consequently, the body needs to produce more insulin to maintain normal blood glucose levels, potentially paving the way for metabolic issues in the long term. This underscores the importance of prioritizing adequate, quality sleep for overall well-being and effective metabolic function.
Quantifying Sleep Loss
The impact of sleep deprivation on insulin sensitivity is not just theoretical; it's backed by research and expert observations. The assertion that a single night of only four hours of sleep can lead to a 25% decrease in insulin sensitivity is a noteworthy claim. This figure gives a clear indication of how quickly and dramatically poor sleep can affect metabolic processes. The body’s response to sleep deprivation is complex, encompassing hormonal changes and alterations in cellular function. It's not merely a matter of feeling tired. The decreased insulin sensitivity means the body struggles more to utilize glucose, which can lead to elevated blood sugar levels. Over time, these elevated levels can contribute to insulin resistance, a condition where cells become increasingly unresponsive to insulin, increasing the risk for metabolic syndrome and type 2 diabetes. Therefore, understanding the scale of the impact—a 25% reduction with just one short night of sleep—highlights the urgency of prioritizing sleep.
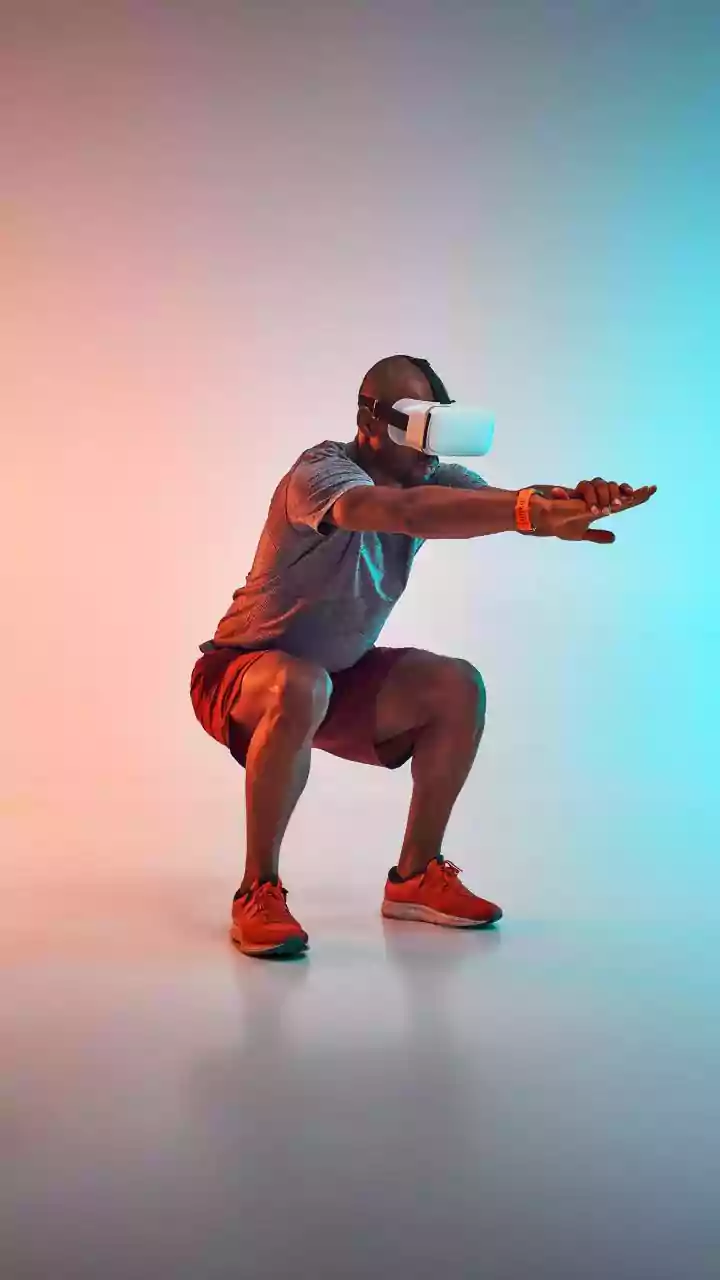
Prioritizing Sleep Habits
Given the significant impact sleep has on insulin sensitivity, it becomes vital to adopt habits that promote better sleep quality. Prioritizing sleep is not just about logging more hours in bed; it also involves setting up a sleep-friendly environment and practicing healthy routines. This could involve establishing a regular sleep schedule, going to bed and waking up at consistent times, even on weekends. Creating a relaxing bedtime routine, such as taking a warm bath or reading a book, can signal to your body that it's time to wind down. Moreover, the bedroom environment plays a critical role. Ensuring the room is dark, quiet, and cool can dramatically improve sleep quality. Limiting exposure to screens and caffeine before bed is also beneficial. By making these changes, individuals can significantly improve their sleep quality, potentially mitigating the negative effects of sleep deprivation on insulin sensitivity, and supporting overall health.
Long-term Metabolic Benefits
The benefits of improved sleep extend far beyond feeling rested; they play a significant role in promoting long-term metabolic health. By consistently prioritizing quality sleep, individuals are supporting the body's ability to effectively process insulin, maintaining healthy blood sugar levels, and lowering the risk of metabolic disorders such as type 2 diabetes. Furthermore, good sleep supports overall cellular function and energy levels. It aids in weight management, as sleep deprivation can disrupt hormones that regulate appetite and hunger. Addressing sleep issues can improve mood, cognitive function, and cardiovascular health. Focusing on improving sleep quality is an investment in long-term health and well-being. It is a proactive step towards building a solid foundation for optimal metabolic function, reducing the risk of chronic diseases, and enhancing quality of life.