What is Celiac Disease?
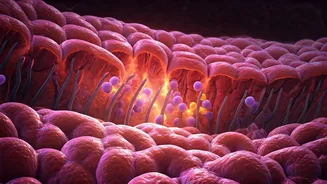
Celiac disease is a significant autoimmune disorder where the consumption of gluten, a protein prevalent in wheat, barley, and rye, provokes an immune system
reaction that specifically targets and damages the small intestine. This chronic condition, while rare, affects approximately 1 in every 100 individuals globally. A notable aspect is that a substantial portion, around 70%, of affected individuals remain undiagnosed, highlighting a gap in awareness and recognition. The immune response in celiac disease is so pronounced that it leads to the erosion of villi, the finger-like projections lining the small intestine responsible for nutrient absorption. This damage severely impairs the body's ability to absorb essential vitamins and minerals, leading to various health complications. Understanding this intricate mechanism is crucial for both diagnosis and management of the condition.
Genetic Predisposition
The genetic makeup of an individual plays a pivotal role in the development of celiac disease. Research indicates a strong hereditary component, with individuals having a first-degree relative diagnosed with the condition facing a significantly increased risk. Specifically, the likelihood of developing celiac disease rises to about 1 in 10 for those with a family history. This genetic susceptibility means that certain individuals are predisposed to developing the autoimmune response when exposed to gluten. While genetics are a primary factor, environmental triggers, such as gluten ingestion, are necessary for the disease to manifest. This highlights the complex interplay between inherited traits and external factors in the onset of celiac disease, emphasizing the importance of family medical history in risk assessment and early detection.
Celiac vs. Gluten Intolerance
It's important to distinguish celiac disease from gluten intolerance, as both conditions can present with similar symptoms but have distinct underlying mechanisms and consequences. While individuals with gluten intolerance may experience adverse reactions to gluten, such as bloating, abdominal pain, or fatigue, their small intestines do not suffer the autoimmune damage characteristic of celiac disease. In gluten intolerance, the immune system is not activated in the same way, and the villi of the small intestine remain intact. This critical difference means that the long-term effects on nutrient absorption and potential for intestinal damage are unique to celiac disease. Proper diagnosis is therefore essential to differentiate between these conditions, as management strategies and potential health risks vary significantly.