For decades, cervical cancer in India has been quietly boxed into a misleading narrative – that it is a disease that concerns only married women. This assumption has done more harm than good. It delays
screening, discourages young women from seeking preventive care, and reinforces silence around sexual health. In reality, cervical cancer has little to do with marital status and everything to do with exposure to a common virus, awareness, and access to timely screening. As India continues to shoulder a significant share of the global cervical cancer burden, breaking this myth becomes urgent.
HPV: The Real Risk Factor
“Cervical cancer is a cancer caused by a viral infection – Human Papillomavirus (HPV). One need not be married to get this infection. Even skin-to-skin contact with an infected person can transmit HPV,” explains Dr Sampada Dessai, Consultant Gynaecological Cancer and Robotic Surgeon at P. D. Hinduja Hospital, Mumbai.
HPV is one of the most common sexually transmitted infections globally, and most people will encounter it at some point in their lives. “HPV infection usually does not cause any symptoms and often clears on its own. But if it persists for a long time, it can eventually lead to cervical cancer,” Dr Dessai adds.
What determines risk, she stresses, is sexual exposure – not marriage. Multiple sexual partners increase risk, while barrier contraception like condoms offers partial protection by limiting direct contact.
Why Awareness Gaps Persist In India
According to Dr Vivekanand Sharma, Consultant Surgical Oncologist at Fortis Hospital, Kalyan, India, cervical cancer still accounts for nearly 20 per cent of global cervical cancer cases and deaths, despite some progress in disease control.
“A large proportion of this burden exists because of lack of awareness, misinformation, and the absence of a nationally established screening programme,” he says. Sexual health conversations remain taboo, often leaving young women uninformed or misinformed.
Dr Sharma points out that while national surveys report low rates of premarital sexual activity, independent studies suggest the numbers may be much higher. “This under-reporting reflects societal barriers to open conversations, not the absence of risk,” he notes.
Screening Saves Lives At Any Age
One of the most effective tools against cervical cancer is early detection. “HPV is common and hard to detect unless tests are taken. Pap smear and HPV DNA testing should be offered to all sexually active women,” says Dr Sharma.
Regular screening helps detect pre-cancerous changes long before cancer develops. Yet many young women delay or avoid tests, believing they are unnecessary before marriage – a misconception both experts strongly caution against.
Dr Dessai reiterates that cervical cancer prevention must begin early. “Marriage is not the criteria. Sexual history is far more relevant when assessing risk,” she says.
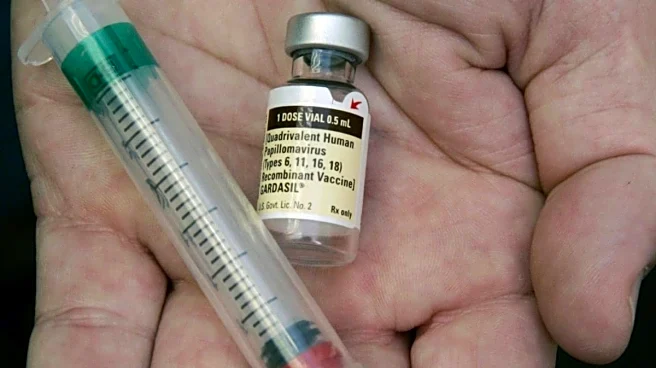
Vaccination: A Critical Preventive Step
HPV vaccination has emerged as a powerful preventive tool, especially when administered on time. “It’s encouraging to see organisations like FOGSI and IAP pushing for increased vaccine uptake,” says Dr Sharma. The development of an indigenous HPV vaccine, he adds, could make prevention more accessible and equitable across India.
Vaccination does not eliminate the need for screening, but together, the two significantly reduce cervical cancer risk.
At its core, cervical cancer prevention is about replacing silence with science. Young women deserve accurate information, access to screening, and freedom from outdated social labels. Parents, schools, healthcare systems, and society at large must normalise conversations around sexual health – without judgment or stigma.



/images/ppid_a911dc6a-image-177100042462595765.webp)

/images/ppid_a911dc6a-image-177100003665395152.webp)
/images/ppid_a911dc6a-image-177100010230548853.webp)
/images/ppid_59c68470-image-177100002975460427.webp)






