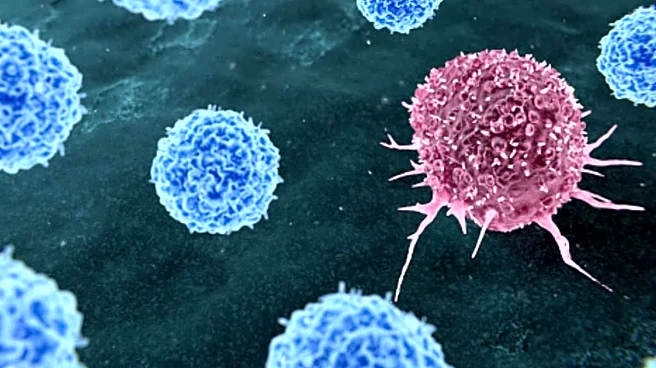
Cervical cancer is often described as one of the most preventable cancers affecting women, yet it continues to pose a serious global health challenge. At its core lies a common and largely silent trigger: persistent infection with high-risk strains of the human papillomavirus, or HPV, a virus most people encounter at some point in their lives. When detected early, cervical cancer is highly treatable but the problem is that it often is not. Missed screenings, delayed evaluations and a tendency to normalise symptoms mean the disease is frequently diagnosed only after it has advanced.
Global health agencies have repeatedly flagged this gap between prevention and reality. A 2026 report by the International Agency for Research on Cancer revealed that
more than 660,000 women were diagnosed with cervical cancer worldwide in 2022, with close to 350,000 deaths recorded the same year. What makes this especially troubling is that the science around prevention is no longer uncertain. A 2025 study by Sweden’s Karolinska Institutet showed that HPV vaccination administered before exposure to the virus can reduce the risk of cervical precancer by more than 50%.
In India, less than 2% of women undergo regular cervical cancer screening, even as incidence rates remain high, particularly in those who reach healthcare only at late stages.
For Nitu, it began with something she didn’t talk about much. A vaginal discharge that felt different from usual heavier, persistent, and uncomfortable in a way she couldn’t explain. Alongside it came a dull discomfort in her lower abdomen, the kind that lingers but never quite announces itself as pain.
At 46, Nitu Kappor a mother of two children moved through the daily demands of life the way many women do— adjusting, coping, managing, and rarely stopping to question the small changes her body was signalling. The symptoms didn’t feel urgent, they just felt inconvenient.
Weeks passed and then months, by December 2024, the symptoms were no longer occasional. They had become part of Nitu’s routine, like a constant background noise she had learned to ignore. There was a reluctance to worry, a belief that these changes were part of getting older or simply something she could handle without medical attention.
But the vaginal discharge persisted with discomfort. In May 2025, she finally sought medical advice. Her family supported her, but there was also a sense of hesitation, a delay that many women experience when symptoms feel private, embarrassing, or “not serious enough.” Still, the discomfort had grown enough to push her to investigate.
When she finally sought medical advice, the imaging results were the first moment her symptoms became more than just discomfort. A contrast-enhanced CT scan done on 27 May 2025 showed a well-defined solid-cystic mass lesion in the left region near the uterus, initially thought to be a tubo-ovarian mass (serious inflammatory collection of pus involving the fallopian tube and ovary). It was a first sign that something serious was happening inside her body.
A follow-up MRI on 2 June 2025 brought clarity and fear in equal measure. The scan revealed a large lobulated mass (small, rounded sections) arising from the cervix, measuring roughly 29 x 19 x 47 mm alomost the size of a large egg, with clear signs of invasion into nearby tissues. The upper vagina was involved, and the mass was closely touching the bladder base. The fat plane between the tumour and the bladder was obscured, and the posterior bladder wall appeared irregularly thickened.
The scan also showed that the tumour was pressing very close to the rectum, and the tissue between them looked disturbed. This suggested it might be starting to spread there. On the sides, the mass had grown into the surrounding tissues of the pelvis.
The ovaries also showed changes. Both had several small lesions, with the left ovary appearing larger and having more cysts. There was also a swollen tube-like structure near the left ovary, likely a hydrosalpinx.
By 9 June 2025, a biopsy confirmed the diagnosis: adenosquamous carcinoma of the cervix, Grade 1. Blood tests showed tumour marker CA125 was rising, from 127 on 30 May to 191 by 14 August, indicating the disease was active and progressing.
And yet, the emotional reality was complicated. She still felt “functional” still managing daily life even as her body was undergoing a silent transformation.
After her diagnosis, Nitu chose to try Ayurvedic treatment, and her family supported her decision. She continued with it for several weeks. This was not necessarily because she rejected medical advice, but because the diagnosis felt overwhelming and hard to accept.
She returned to the oncology clinic in September 2025, and again on 4 November 2025. During this time, the disease continued to grow. A detailed MRI scan in October 2025 showed that the tumour had grown larger, now measuring 54 × 33 × 30 mm almost the size of a matchbox. It had spread into the upper part of the vagina and was reaching the mid-body of the uterus. The scan also showed it was very close to the bladder and might be starting to affect the rectum.
The cancer had also spread to nearby lymph nodes. Several lymph nodes in the pelvic area were enlarged, and the largest was about 11 mm. Both fallopian tubes were filled with blood (a condition called hematosalpinx), and the left ovary appeared larger with multiple cysts.
A PET-CT scan showed that the cervical tumour was active and spreading. It also found a large mass in the left ovary area, which could be either a spread of the cancer or a new tumour. The scan also showed cancer activity in several lymph nodes in the pelvis and near the aorta.
Facing advanced disease, the medical team outlined a multimodal treatment strategy. The plan began with induction chemotherapy using Pacliaqualip (a paclitaxel formulation) plus carboplatin administered weekly over six weeks, followed by concurrent chemoradiotherapy (CCRT).
Dr Jyoti Wadhwa, Director of Medical Oncology at Apollo Athenaa Women’s Cancer Centre and the lead physician managing this case emphasises the importance of coordinated care. “When cervical cancer spreads beyond the cervix, symptoms often become more noticeable,” she says. “Persistent pelvic or lower abdominal pain, back pain, abnormal vaginal bleeding, foul-smelling or watery discharge, difficulty passing urine or stools, swelling of the legs, fatigue and unexplained weight loss are signs that should never be ignored. Prompt medical evaluation can make a crucial difference.”
She points out that symptom interpretation often varies among women. “Many women dismiss early changes as routine or related to non-serious conditions. But signs like persistent discharge especially if blood-stained or foul-smelling and pelvic discomfort lasting more than two to three weeks should trigger urgent evaluation.”
Surgery remains a central treatment for early cervical cancer confined strictly to the cervix. But in this case, and in many advanced ones like it, the disease has breached tissue margins and involved lymphatic spread, making complete surgical removal unlikely. “When cancer infiltrates surrounding tissues, lymph nodes or nearby organs, surgery alone cannot eradicate all disease safely,” Dr Wadhwa explains. “Chemotherapy combined with radiation offers better control and improves the chances of response and survival.”
For patients anxious about treatment side effects like hair loss, nausea, fatigue modern oncology practice offers targeted support. “We now have effective medicines to control nausea and vomiting, and approaches like scalp cooling can reduce hair loss,” Dr Wadhwa says. “Fatigue is monitored and managed, and we encourage patients to speak openly about their concerns. Most side effects are temporary and manageable.”
Understanding the biological behaviour of the tumour also helps personalise care. In Nitu’s case, hormone receptor positivity suggests that cancer cells respond to certain body hormones, a factor that may guide future treatment decisions, even if it does not alter the standard first-line approach. Dr Wadhwa explains the significance succinctly, “A hormone-sensitive cancer has cells that respond to natural hormones in the body. Identifying this helps doctors personalise treatment and plan long-term care more effectively. While it does not change the need for standard treatment, it can guide future therapeutic decisions.”
Despite the fact that cervical cancer is highly preventable, it remains a leading cause of cancer death among women in many parts of the world. “In many countries, cervical cancer should no longer be a major killer because of vaccination against HPV and regular screening,” says Dr Wadhwa. But barriers — social, cultural and logistical continue to limit access to these interventions.
Dr Wadhwa reiterates that any persistent change, particularly in women over 40, warrants evaluation. “Any persistent vaginal discharge, especially if it is foul-smelling, watery, blood-stained, or new after the age of 40, needs urgent medical attention. Similarly, lower abdominal or pelvic discomfort lasting more than two to three weeks, or associated with bleeding, urinary, or bowel symptoms, should not be dismissed as routine. Early evaluation can save lives.”



/images/ppid_59c68470-image-17707051657521865.webp)

/images/ppid_a911dc6a-image-177063883543242302.webp)

/images/ppid_a911dc6a-image-177062770230616253.webp)


/images/ppid_a911dc6a-image-177057403153775600.webp)