What's Happening?
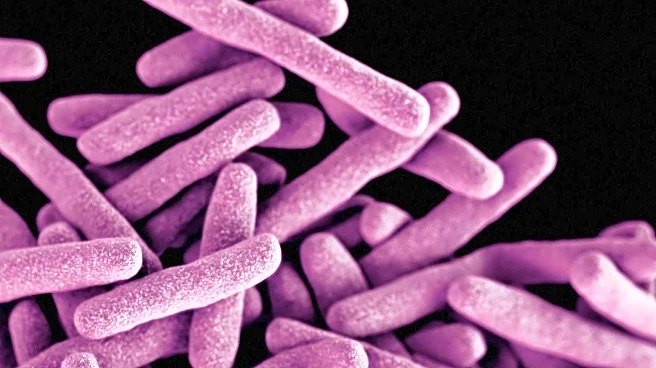
Recent research highlights the potential of microbiome profiling as a non-invasive diagnostic tool for neuropsychiatric conditions in elderly patients. The studies reviewed focus on the gut microbiome's influence on brain function, particularly in conditions like
Alzheimer's and Parkinson's diseases, as well as psychiatric disorders such as depression and schizophrenia. The gut microbiome can affect neuropsychiatric health through mechanisms like immune modulation and microbial metabolite release. While current evidence supports an association between microbiome changes and neuropsychiatric conditions, causality has not been established. The research suggests that microbiome profiling could help stratify patients into specific subgroups, aiding in more precise diagnoses and targeted treatments. However, challenges remain, such as the overlap of microbial features across different conditions, which may limit diagnostic specificity.
Why It's Important?
The integration of microbiome profiling into clinical practice could revolutionize the diagnosis and treatment of neuropsychiatric conditions in the elderly. By providing a less invasive and potentially more cost-effective alternative to current diagnostic methods like neuroimaging, this approach could improve accessibility and timeliness of care. The ability to predict treatment responsiveness and disease progression through microbiome data could lead to more personalized and effective interventions. This development is particularly significant given the aging U.S. population and the increasing prevalence of neuropsychiatric disorders. However, the need for larger, more diverse studies and standardized methodologies highlights the ongoing challenges in translating these findings into clinical practice.
What's Next?
Future research is expected to focus on establishing causality through long-term studies and improving diagnostic specificity by distinguishing between overlapping conditions. The use of advanced sequencing techniques and machine learning in data analysis is likely to enhance the accuracy and applicability of microbiome-based models. Additionally, broader multiomics approaches, incorporating metatranscriptomics and metabolomics, may provide deeper insights into the microbiome's role in neuropsychiatric health. As the field progresses, the development of standardized tools and larger, multicenter studies will be crucial in validating these models for clinical use.
Beyond the Headlines
The ethical and practical implications of microbiome profiling in healthcare are significant. As this technology advances, issues such as data privacy, consent, and the potential for misuse of genetic information will need to be addressed. Furthermore, the integration of microbiome data into healthcare systems may require new regulatory frameworks and training for healthcare professionals. The potential for microbiome profiling to contribute to precision medicine also raises questions about healthcare equity and access, particularly for underserved populations.