What's Happening?
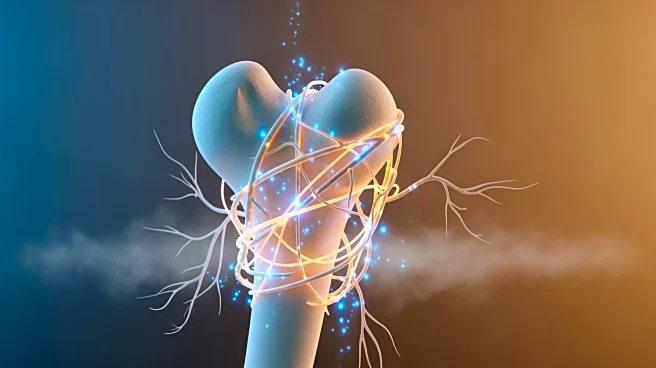
Recent research has uncovered a critical role for neutrophils in bone healing, specifically through the initiation of nociceptive nerve ingrowth. This process is crucial for resolving inflammation and
promoting bone regeneration. The study, conducted using a murine femoral diaphysis defect model, observed that TRPV1+ nociceptive fibers begin to extend early in the healing process, peaking around day 7 post-injury. This nerve growth coincides with a decrease in inflammation, as indicated by reduced levels of interleukin-1β (IL-1β), a key inflammatory mediator. The study further demonstrated that nociceptive innervation acts as a regulatory mechanism, restraining inflammation during the early stages of bone healing. Ablation of these nociceptors led to increased inflammatory cytokines and impaired bone regeneration, highlighting their importance in the healing process.
Why It's Important?
The findings of this study have significant implications for understanding the mechanisms of bone healing and inflammation resolution. By elucidating the role of nociceptive nerve fibers in regulating inflammation, this research could inform new therapeutic strategies for enhancing bone regeneration, particularly in conditions characterized by chronic inflammation or impaired healing. The ability to modulate nociceptive innervation could lead to improved outcomes in bone repair and recovery, potentially benefiting patients with fractures, osteoporosis, or other bone-related conditions. Furthermore, this study underscores the complex interplay between the nervous and immune systems in tissue regeneration, opening avenues for interdisciplinary research and treatment approaches.
What's Next?
Future research may focus on developing targeted therapies that enhance nociceptive nerve growth or mimic its effects to promote bone healing. Such therapies could involve the use of growth factors, nerve stimulators, or other agents that facilitate the resolution of inflammation and support tissue regeneration. Additionally, clinical trials may be necessary to evaluate the safety and efficacy of these potential treatments in human patients. Understanding the molecular pathways involved in nociceptive innervation and inflammation resolution could also lead to the identification of new drug targets for bone-related diseases.
Beyond the Headlines
This study highlights the broader implications of neuro-immune interactions in tissue healing and regeneration. The findings suggest that the nervous system plays a more active role in immune regulation than previously thought, potentially influencing a wide range of inflammatory and degenerative conditions. The concept of using nerve growth modulation as a therapeutic strategy could extend beyond bone healing to other areas of regenerative medicine, such as wound healing, organ repair, and even cancer treatment, where inflammation plays a critical role.