What's Happening?
A recent case at Fortis Hospital, Mohali, highlights the dangers of antibiotic misuse, as a young man suffered massive intestinal bleeding due to self-medication with ciprofloxacin. This incident underscores
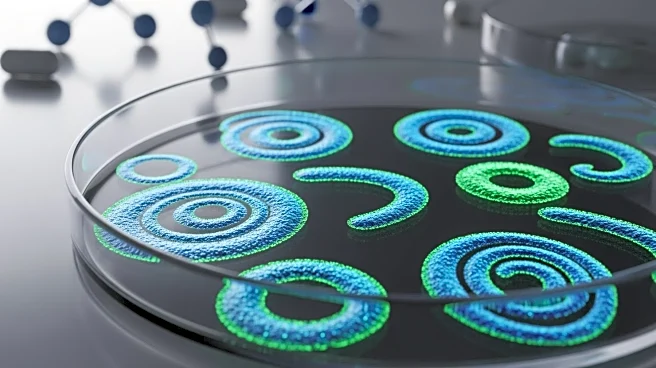
the growing problem of antimicrobial resistance (AMR), where microorganisms evolve to withstand drugs designed to kill them. The misuse of antibiotics, particularly over-the-counter sales and self-medication, contributes significantly to this issue. According to Dr. Parvinder Chawla, senior consultant in Internal Medicine, typhoid is a glaring example of AMR, with ciprofloxacin becoming ineffective due to unsupervised use. A study published in The Lancet reveals that India has the highest global prevalence of multidrug-resistant organisms among patients undergoing common endoscopic procedures, with 83.1% carrying at least one superbug.
Why It's Important?
The rise of antimicrobial resistance poses a significant threat to public health, making infections harder to treat and increasing the risk of prolonged illness and death. In India, the misuse of antibiotics has led to a high prevalence of multidrug-resistant organisms, complicating treatment protocols and increasing healthcare costs. This situation demands urgent action to prevent, diagnose, and treat infections effectively. Healthcare professionals are urged to educate themselves on responsible antibiotic use and implement measures for infection prevention, such as hand hygiene and vaccination. Failure to address AMR could lead to common infections becoming fatal, impacting public health and the healthcare system.
What's Next?
Healthcare professionals and policymakers must prioritize antimicrobial stewardship to combat the rise of AMR. This includes rationalizing antibiotic use, improving infection prevention measures, and educating the public on the dangers of self-medication. Hospitals may need to revise treatment protocols, opting for intravenous antibiotics for suspected typhoid cases. Continued research and monitoring of resistance patterns are essential to adapt strategies and prevent further escalation of AMR. Collaborative efforts between healthcare providers, government agencies, and the public are crucial to mitigate this growing threat.
Beyond the Headlines
The implications of antimicrobial resistance extend beyond immediate health risks, potentially affecting global healthcare systems and economies. As resistance patterns evolve, the development of new antibiotics and treatment methods becomes increasingly urgent. Ethical considerations arise regarding the accessibility and affordability of effective treatments, particularly in low-income regions. Long-term shifts in healthcare practices, including stricter regulations on antibiotic sales and enhanced public health campaigns, may be necessary to curb the spread of resistant strains.