What's Happening?
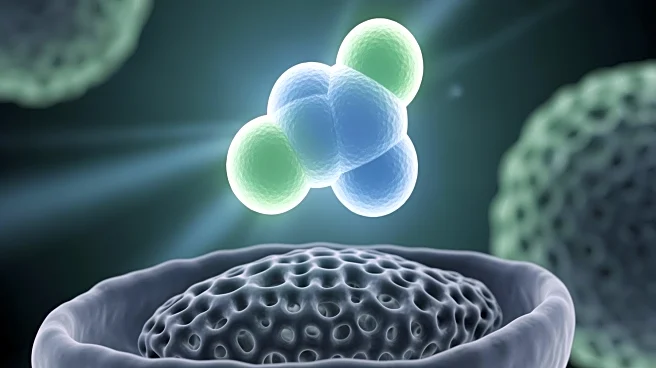
Recent research has highlighted the role of a microbiota-dependent bile acid, isolithocholic acid (isoLCA), in modulating lung immunity. The study involved experiments on mouse primary lung immune cells
and human monocyte-derived macrophages (MDMs). These cells were stimulated with lipopolysaccharide (LPS) in the presence of isoLCA, which resulted in a significant modulation of the pro-inflammatory response. The experiments demonstrated that isoLCA could influence the expression of CXCL10, a chemokine involved in immune responses, and alter the influx of neutrophils into the lungs. The study also explored the expression of bile acid receptors in human MDMs and the impact of isoLCA on mitochondrial membrane potential and lactate secretion. These findings suggest that isoLCA has the potential to reprogram alveolar macrophages, thereby controlling lung inflammation.
Why It's Important?
The discovery of isoLCA's role in modulating lung immunity is significant as it opens new avenues for treating inflammatory lung diseases. By understanding how microbiota-derived metabolites like isoLCA can influence immune responses, researchers can develop targeted therapies for conditions such as asthma and chronic obstructive pulmonary disease (COPD). This research underscores the importance of the microbiota in systemic immunity and highlights the potential for microbiota-derived compounds to serve as therapeutic agents. The ability to control lung inflammation through such compounds could lead to more effective and less invasive treatments, reducing the reliance on traditional anti-inflammatory drugs that often come with significant side effects.
What's Next?
Future research will likely focus on further elucidating the mechanisms by which isoLCA and similar compounds exert their effects on immune cells. Clinical trials may be initiated to test the efficacy and safety of isoLCA-based treatments in humans. Additionally, researchers may explore the potential of other microbiota-derived metabolites in modulating immune responses in different tissues. The development of new therapeutic strategies based on these findings could revolutionize the treatment of inflammatory diseases, offering more personalized and precise medical interventions.
Beyond the Headlines
This research highlights the broader implications of microbiota-derived metabolites in systemic health. The ability of these compounds to influence immune responses at distal sites suggests a complex interplay between the gut microbiota and overall immune function. This could lead to a paradigm shift in how we understand and treat diseases, emphasizing the role of the microbiome in health and disease. Furthermore, the ethical considerations of manipulating the microbiome for therapeutic purposes will need to be addressed, ensuring that such interventions are safe and effective.