What's Happening?
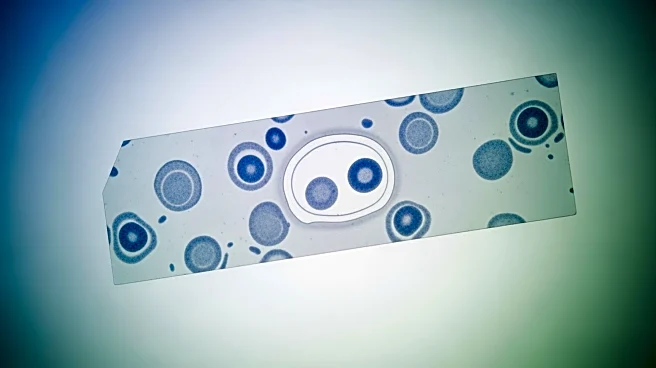
A recent study has identified a significant association between monocyte percentage (MP) and chronic endometritis (CE) in infertile patients. The research, conducted as a cross-sectional study, found that MP levels were inversely correlated with the incidence
of CE. Monocytes, which are crucial components of the innate immune system, play a role in inflammation and immune response. The study suggests that elevated monocyte levels may occur earlier in the inflammatory process, potentially serving as an early marker for CE. This finding could provide a non-invasive, cost-effective method for early screening of CE in infertile women, as MP can be measured through routine blood tests. The study also highlights the potential of MP as a prognostic tool, reflecting CE activity and therapeutic response.
Why It's Important?
The study's findings are significant as they offer a new approach to diagnosing and managing chronic endometritis, a condition that can affect fertility. By identifying monocyte percentage as a potential early marker for CE, healthcare providers could improve early detection and intervention strategies, potentially enhancing fertility outcomes for affected women. The ability to use a simple blood test for early screening could reduce the need for invasive procedures like endometrial biopsies, making the process more accessible and less burdensome for patients. Additionally, understanding the role of monocytes in CE could lead to more targeted treatments, improving patient care and outcomes in reproductive health.
What's Next?
Future research is needed to validate these findings across larger, diverse populations and to explore the underlying immunological mechanisms. Prospective studies could establish clinical cutoff values for MP and investigate its utility in predicting treatment responses and fertility outcomes. There is also potential for developing multi-marker panels that combine MP with other biomarkers to enhance diagnostic and prognostic capabilities. Such advancements could lead to standardized, automated processes for clinical implementation, ultimately improving the management of chronic endometritis in infertile patients.