What's Happening?
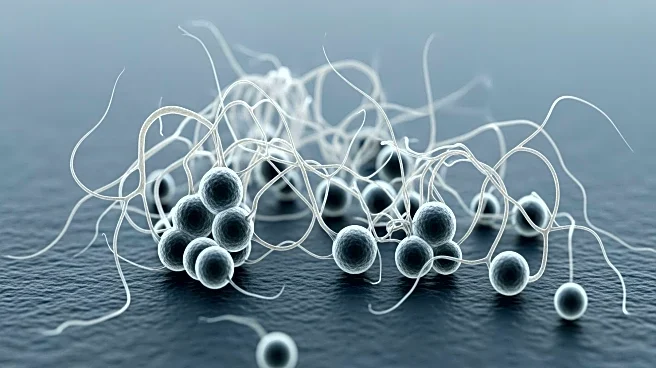
A study conducted by the Leibniz Institute for Natural Product Research and Infection Biology has uncovered a dangerous alliance between the yeast Candida albicans and the bacterium Enterococcus faecalis. These microorganisms, typically harmless inhabitants
of human mucous membranes, can cause severe infections when the immune system is compromised or the microbial balance is disturbed. The research, published in the Proceedings of the National Academy of Sciences, highlights the role of the bacterial toxin cytolysin in this interaction. Cytolysin, produced by certain strains of E. faecalis, perforates cell membranes, leading to increased cell damage when combined with Candida albicans. The study found that direct contact between the bacteria and fungi, along with nutrient depletion by the fungus, exacerbates the damage to host cells.
Why It's Important?
This discovery is significant as it sheds light on the complex interactions between different microorganisms that can lead to severe infections. Understanding these interactions is crucial for developing targeted therapies to combat such infections, especially in individuals with weakened immune systems. The findings emphasize that the severity of an infection is not solely dependent on a single microorganism but on the combination of microbes and their interactions. This knowledge could lead to more effective treatments and preventive measures against infections caused by microbial alliances, potentially reducing the burden on healthcare systems and improving patient outcomes.
What's Next?
Future research may focus on developing therapies that target the specific interactions between Candida albicans and Enterococcus faecalis, particularly those involving cytolysin. By understanding the mechanisms of these interactions, scientists could create interventions that disrupt the harmful alliance, thereby reducing infection severity. Additionally, further studies could explore other microbial interactions that contribute to disease, broadening the scope of infection control strategies. Healthcare providers might also consider these findings when treating patients with compromised immune systems, potentially adjusting treatment protocols to address the risk of combined infections.
Beyond the Headlines
The study highlights the importance of considering microbial interactions in the context of infection control and treatment. It challenges the traditional view of treating infections caused by single pathogens, suggesting a more holistic approach that accounts for microbial communities. This perspective could lead to a paradigm shift in how infections are diagnosed and managed, emphasizing the need for comprehensive microbial profiling in clinical settings. Moreover, the research underscores the potential for microbial interactions to influence the evolution of pathogenicity, raising questions about the long-term implications for public health and disease prevention.