What's Happening?
A recent study conducted at Shanghai Children’s Medical Center has identified key clinical, endoscopic, and histopathological markers for diagnosing pediatric gastrointestinal graft-versus-host disease
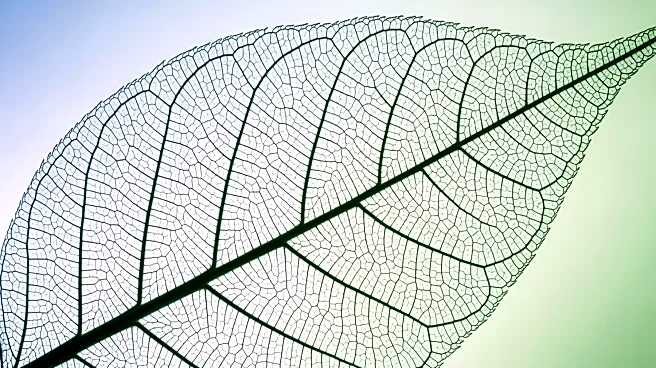
(GI-GVHD). The research involved a retrospective analysis of post-bone marrow stem cell transplant patients with gastrointestinal symptoms from 2018 to 2023. The study found that GI-GVHD was associated with symptoms such as skin rejection, diarrhea, and bloody stools. Notably, the study highlighted the significance of transverse colonic mucosal edema and tortoise shell-like mucosa as indicators of GI-GVHD. These findings were used to develop a nomogram prediction model, which combines gastroscopy and colonoscopy for improved diagnostic accuracy.
Why It's Important?
The study's findings are crucial for enhancing the early and accurate diagnosis of GI-GVHD in pediatric patients, which can lead to timely and targeted interventions. This is particularly important as GI-GVHD can significantly impact the quality of life and overall health outcomes of affected children. By identifying specific markers and developing a predictive model, healthcare providers can better assess the risk and presence of GI-GVHD, potentially reducing the morbidity associated with this condition. The research underscores the importance of comprehensive diagnostic approaches in managing complex post-transplant complications.
What's Next?
The introduction of the nomogram prediction model is expected to influence clinical practices by providing a more structured approach to diagnosing GI-GVHD. Healthcare institutions may adopt this model to improve diagnostic protocols, potentially leading to better patient management and outcomes. Further research could explore the application of this model in different populations and settings, as well as its integration into routine clinical practice. Additionally, ongoing studies may focus on refining the model and exploring other potential markers for GI-GVHD.
Beyond the Headlines
The study also raises awareness about the complexities of post-transplant care in pediatric patients. It highlights the need for continuous advancements in diagnostic techniques to address the unique challenges faced by this vulnerable population. The findings may prompt discussions on the allocation of resources towards research and development in pediatric transplant care, emphasizing the importance of innovation in improving patient outcomes.