What's Happening?
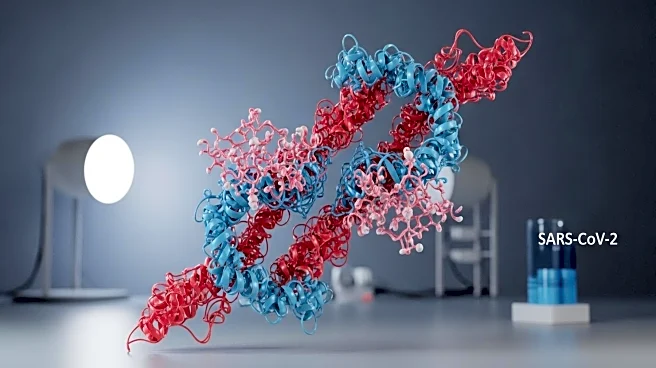
Scientists at Scripps Research have conducted an siRNA screen to identify human proteins that SARS-CoV-2 uses for its replication cycle. This research, published in PLOS Biology, highlights dozens of host proteins that could be targeted to develop new treatments for COVID-19 and other coronaviruses. The study uncovered 32 proteins essential for early infection stages and 27 for later stages, along with several cellular pathways exploited by the virus. Two proteins, perlecan and BIRC2, emerged as promising drug targets. Perlecan acts as a co-receptor for the virus, while BIRC2 is involved in cellular inflammation pathways. The findings suggest potential for pan-coronavirus therapies that target host proteins, reducing the risk of drug resistance due to viral mutations.
Why It's Important?
The identification of host proteins critical to SARS-CoV-2 replication offers a new avenue for antiviral drug development. By targeting these proteins, researchers can potentially create treatments effective against multiple coronaviruses, including future variants. This approach could mitigate the challenges posed by viral mutations and drug resistance, providing a more robust defense against pandemics. The research also opens possibilities for developing broad-spectrum antivirals that could be deployed early in future outbreaks, enhancing preparedness and response capabilities.
What's Next?
Researchers plan to investigate whether the identified host proteins are also utilized by other respiratory pathogens like influenza and RSV. Further studies will focus on testing the safety and efficacy of promising compounds targeting these proteins. The goal is to develop antivirals that can be rapidly deployed in response to new coronavirus outbreaks, potentially blocking multiple viruses with a single therapy.
Beyond the Headlines
The study's approach to targeting host proteins rather than the virus itself represents a shift in antiviral strategy, emphasizing the importance of understanding host-pathogen interactions. This could lead to long-term changes in how infectious diseases are treated, prioritizing therapies less susceptible to resistance and adaptable to evolving pathogens.