What's Happening?
The Mammo-50 trial, a multicenter, randomized, phase 3 study, investigates the cost-effectiveness of annual versus less frequent mammographic surveillance in women aged 50 and older who have been treated for breast cancer. Participants were eligible if
they had undergone curative surgery and showed no recurrence for three years post-treatment. The trial included women with invasive breast cancer or ductal carcinoma in situ (DCIS), excluding those with bilateral breast cancer, known high-risk genetic mutations, or previous malignancies. The study performed two economic evaluations: a within-trial analysis assessing the cost-effectiveness of annual mammography compared to less frequent surveillance over five years, and a budget impact analysis estimating potential NHS savings from reduced-frequency surveillance. The trial collected comprehensive data on hospital resource use, health-related quality of life, and societal costs, using multiple imputation to address missing data.
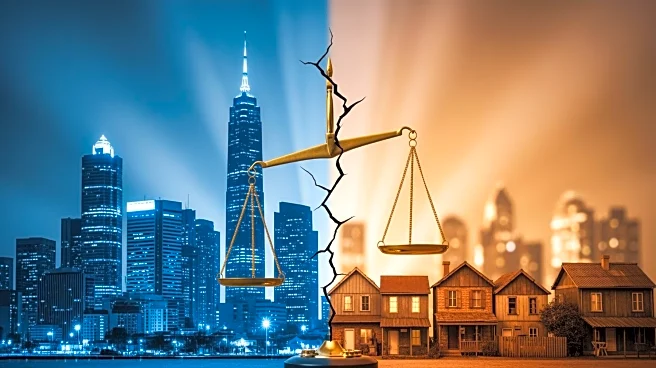
Why It's Important?
This trial is significant as it addresses the economic implications of mammographic surveillance frequency in older breast cancer patients, potentially influencing healthcare policy and resource allocation within the NHS. By evaluating the cost-effectiveness of less frequent surveillance, the study could lead to substantial savings for the healthcare system, while maintaining patient care quality. The findings may impact decisions on surveillance protocols, balancing cost savings with patient outcomes. Stakeholders, including healthcare providers and policymakers, stand to benefit from insights into optimizing surveillance strategies, potentially improving resource management and patient care efficiency.
What's Next?
The trial's results could prompt a reevaluation of current surveillance guidelines, potentially leading to policy changes that favor less frequent mammography for certain patient groups. Healthcare providers may need to adjust their practices based on new recommendations, while policymakers could consider implementing these findings to achieve cost savings. Further research may be conducted to explore the long-term impacts of reduced surveillance frequency on patient outcomes and healthcare costs. Stakeholders will likely monitor the trial's outcomes to assess its applicability to broader patient populations and healthcare systems.
Beyond the Headlines
The Mammo-50 trial highlights ethical considerations in balancing cost-effectiveness with patient care quality. It raises questions about the optimal frequency of surveillance that ensures patient safety without unnecessary healthcare expenditure. The study may influence cultural perceptions of cancer surveillance, encouraging a shift towards personalized care strategies. Long-term, the trial could contribute to a paradigm shift in how healthcare systems approach cancer surveillance, emphasizing evidence-based practices that prioritize both economic and patient-centered outcomes.