What's Happening?
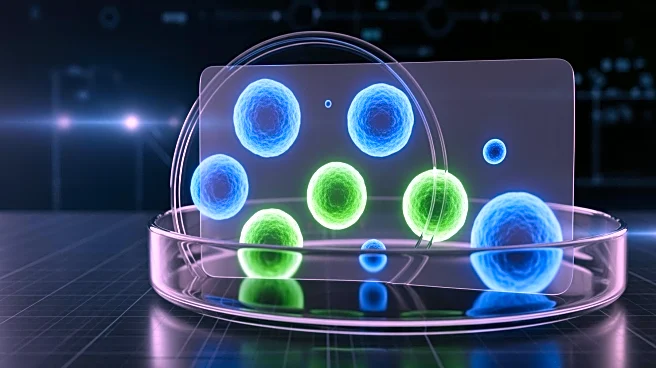
A recent study published in JAMA Network Open highlights the significant impact of discrimination and chronic stress on the lifespan of Black Americans. Conducted by researchers at Washington University in St. Louis, the study tracked over 1,500 Black and White
adults in the St. Louis area over 17 years. It found that nearly half of the mortality gap between Black and White adults can be attributed to the cumulative effects of stress and inflammation. The study focused on two proteins, C-reactive protein and interleukin-6, which are linked to inflammation and tend to linger in the blood after repeated activation of the body's fight-or-flight response. The findings support the 'weathering hypothesis,' which suggests that the biological wear and tear from overcoming societal hardships contributes to health disparities.
Why It's Important?
This study underscores the profound impact of systemic racism and discrimination on health outcomes, particularly for Black Americans. By linking chronic stress and inflammation to earlier mortality, the research provides empirical evidence of how societal inequities manifest in physical health disparities. The findings highlight the need for policy interventions that address the root causes of these disparities, such as economic hardship, discrimination, and lack of access to healthcare. The study also emphasizes the importance of considering everyday stressors, such as microaggressions and the need for code-switching, which contribute to the physiological toll on marginalized communities. This research could inform public health strategies aimed at reducing health inequities and improving the overall well-being of Black Americans.
What's Next?
While the study provides critical insights into the biological impact of discrimination, it does not specify the structural forms of racism that contribute to these health disparities. Future research could focus on identifying specific societal factors, such as redlining, income inequality, and school segregation, that exacerbate health inequities. Additionally, there is a need for policy changes that address these systemic issues and promote health equity. Health equity experts suggest that the study's findings may not immediately influence policy due to its broad focus, but it adds to the growing body of evidence advocating for comprehensive interventions to address racial health disparities.
Beyond the Headlines
The study's findings highlight the broader implications of systemic racism on public health. It challenges the notion that stress management alone can mitigate the health impacts of discrimination, emphasizing the need for structural changes to address the root causes of health inequities. The research also points to the potential for biomarkers to serve as indicators of stress-related health risks, which could be used to develop targeted interventions. However, the study's limitations, such as its focus on major stress events rather than daily stressors, suggest that further research is needed to fully understand the complex interplay between discrimination, stress, and health outcomes.