What's Happening?
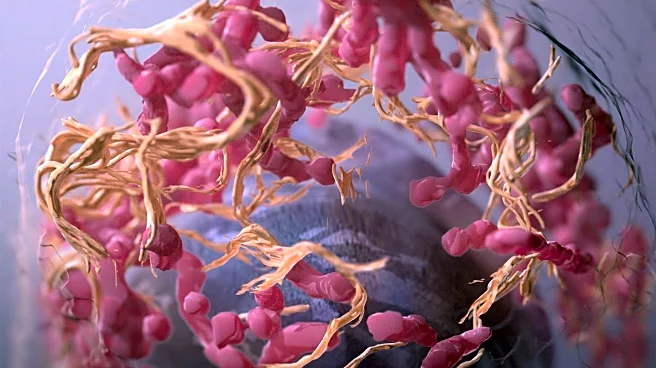
Sana Biotechnology, based in Seattle, Washington, has achieved a significant milestone in diabetes treatment by implanting CRISPR-edited pancreas cells into a person with type 1 diabetes. These cells have successfully produced insulin for several months without requiring the recipient to take immune-suppressing drugs. The gene edits allow the cells, sourced from a deceased donor, to evade detection by the recipient's immune system. This development offers hope for a long-term cure for type 1 diabetes, a condition that affects millions and necessitates constant monitoring and insulin injections. The approach involves immune-cloaking gene edits applied to stem cells, which are then developed into insulin-secreting islet cells. Although the study involved only one person and a low dose of cells, the demonstration of immune cloaking is considered a major milestone toward effective cell therapy without chronic immunosuppression.
Why It's Important?
The advancement in CRISPR-edited cell therapy for diabetes represents a potential breakthrough in medical treatment, offering a path to insulin independence for patients with type 1 diabetes. This could significantly reduce the need for lifelong insulin injections and the associated health risks of immune-suppressing drugs, such as infections and cancer. The ability to evade immune detection could lead to more widespread adoption of cell therapies, addressing the scarcity of donor pancreases and improving patient outcomes. Companies like Vertex Pharmaceuticals and Reprogenix Bioscience are also exploring stem-cell technologies to generate replacement islets, indicating a growing interest in innovative solutions for diabetes management.
What's Next?
Sana Biotechnology's approach may pave the way for further clinical trials and regulatory approval processes. As the technology develops, it could lead to more comprehensive studies involving larger patient groups to establish clinical efficacy and safety. The success of this method could encourage other biotechnology firms to invest in similar immune-cloaking strategies, potentially revolutionizing the treatment landscape for autoimmune diseases. Stakeholders, including healthcare providers and patients, will likely monitor these developments closely, anticipating new treatment options that could improve quality of life and reduce healthcare costs.
Beyond the Headlines
The ethical implications of gene editing in medical treatments are significant, raising questions about the long-term effects and potential risks of altering human cells. As CRISPR technology becomes more prevalent, discussions around regulatory frameworks and ethical guidelines will be crucial to ensure safe and equitable access to these therapies. Additionally, the success of immune-cloaking strategies could influence research in other areas of regenerative medicine, potentially leading to breakthroughs in treating various autoimmune conditions.