What is the story about?
What's Happening?
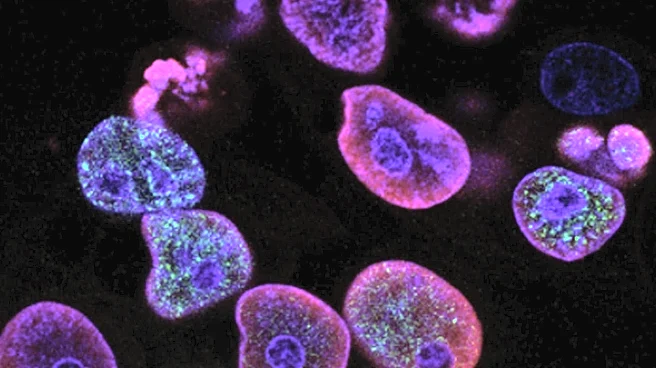
Recent research has highlighted the role of PD-1+ T cells in the development of atherosclerosis. The study focused on the expression of immune checkpoint receptors on T cells, particularly PD-1, which is known to be involved in immune regulation. The research utilized hypercholesterolemic mice models to investigate the presence and behavior of PD-1+ T cells in atherosclerotic aortas. Findings revealed that these T cells exhibit a 'progenitor exhausted' phenotype, characterized by the expression of PD-1 and other markers of T cell exhaustion. The study also noted that PD-1+ T cells in the aorta are associated with increased production of IFNγ, a cytokine linked to inflammation. This suggests that PD-1+ T cells may contribute to the inflammatory processes underlying atherosclerosis.
Why It's Important?
The identification of PD-1+ T cells as contributors to atherosclerosis has significant implications for understanding the disease's pathogenesis and potential treatment strategies. Atherosclerosis is a leading cause of cardiovascular diseases, which are major health concerns in the U.S. The study's findings could pave the way for new therapeutic approaches targeting PD-1+ T cells to mitigate inflammation and slow the progression of atherosclerosis. This could benefit patients by reducing the risk of heart attacks and strokes, which are often caused by atherosclerotic plaque buildup. Additionally, the research underscores the complex role of immune cells in chronic diseases, highlighting the potential for immune-modulating therapies in cardiovascular health.
What's Next?
Future research may focus on developing therapies that specifically target PD-1+ T cells to reduce their inflammatory impact in atherosclerosis. Clinical trials could be designed to test the efficacy and safety of such treatments in human patients. Additionally, further studies might explore the broader implications of immune checkpoint inhibition in cardiovascular diseases, potentially leading to novel interventions that could improve patient outcomes. Researchers may also investigate the role of PD-1+ T cells in other inflammatory conditions, expanding the understanding of immune regulation in chronic diseases.
Beyond the Headlines
The study raises important questions about the balance between immune regulation and inflammation in chronic diseases. While PD-1 is typically associated with immune suppression, its role in promoting inflammation in atherosclerosis suggests a dual function that could be context-dependent. This highlights the complexity of immune checkpoint pathways and their potential as therapeutic targets. Ethical considerations may arise regarding the manipulation of immune responses, particularly in patients with coexisting conditions that could be affected by immune modulation.