What is the story about?
What's Happening?
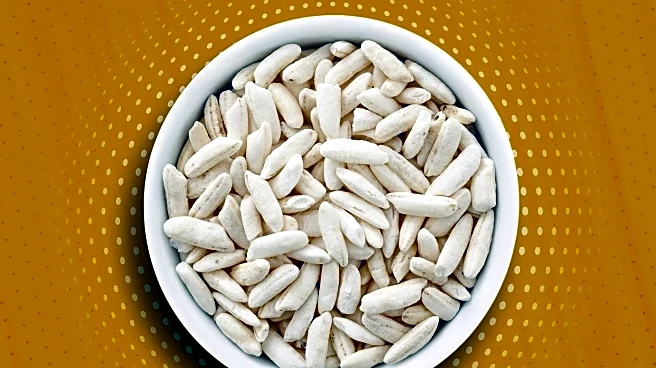
A cross-sectional study conducted at Danderyd Hospital in Stockholm has examined the associations between intestinal microbiota, plasma bile acids, and inflammation markers in patients with Crohn’s disease and ulcerative colitis. The study involved 1,257 participants, with findings indicating significant differences in microbiota composition between IBD patients and controls. The research utilized metagenomic sequencing and bile acid profiling to explore these associations, aiming to better understand the role of microbiota in IBD pathogenesis.
Why It's Important?
Understanding the relationship between intestinal microbiota and inflammation in IBD patients could lead to improved diagnostic and therapeutic strategies. This study highlights the potential for microbiota-targeted interventions to manage IBD symptoms and reduce inflammation. The findings may also contribute to the development of personalized medicine approaches, tailoring treatments based on individual microbiota profiles.
What's Next?
Further research is needed to explore the causal relationships between microbiota composition and inflammation in IBD. Longitudinal studies could provide insights into how microbiota changes over time and its impact on disease progression. Additionally, clinical trials testing microbiota-modulating therapies could offer new treatment options for IBD patients.
Beyond the Headlines
The study raises questions about the ethical considerations of microbiota-based treatments, including the potential risks and benefits of altering gut microbiota. As research progresses, it will be important to address these issues to ensure safe and effective use of microbiota-targeted therapies.