What's Happening?
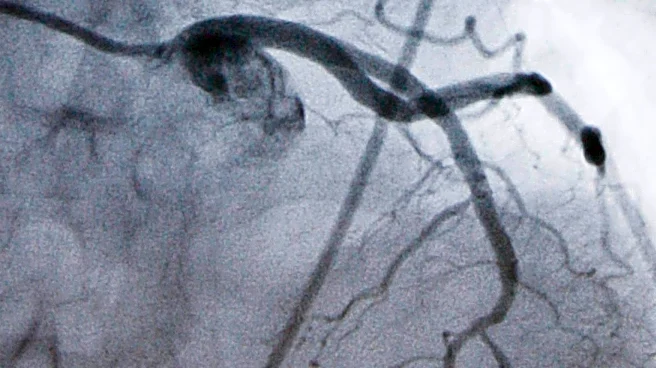
Recent guidelines from major health organizations, including the 2025 American Heart Association (AHA), 2024 European Society of Cardiology (ESC), 2023 European Society of Hypertension (ESH), and 2025 Japanese Society of Hypertension (JSH), emphasize
the critical role of blood pressure (BP) management in stroke care. These guidelines recommend specific BP targets for different types of strokes, such as acute ischemic stroke and intracerebral hemorrhage. For acute ischemic stroke without reperfusion therapy, antihypertensive treatment is advised only if systolic BP is 220 mmHg or higher, or diastolic BP is 120 mmHg or higher. In cases involving reperfusion therapies like thrombolysis, BP should be reduced to below 185/110 mmHg before treatment and maintained below 180/105 mmHg for the first 24 hours. The guidelines also provide recommendations for chronic stroke management, suggesting BP targets of less than 130/80 mmHg to prevent recurrence.
Why It's Important?
These guidelines are crucial as they provide a standardized approach to managing BP in stroke patients, which is a significant factor in improving outcomes and reducing the risk of recurrence. Stroke is a leading cause of death and disability, and effective BP management can significantly impact patient recovery and long-term health. By aligning recommendations across major health organizations, these guidelines aim to reduce variability in treatment and improve patient care globally. The emphasis on specific BP targets helps healthcare providers make informed decisions, potentially reducing the incidence of complications associated with both ischemic and hemorrhagic strokes.
What's Next?
Healthcare providers are expected to integrate these guidelines into clinical practice, which may involve updating treatment protocols and training staff on the new recommendations. Hospitals and clinics might also need to invest in monitoring equipment to ensure accurate BP management. As these guidelines are implemented, further research may be conducted to assess their impact on patient outcomes and to refine recommendations based on emerging evidence. Additionally, patient education will be crucial to ensure adherence to prescribed BP management strategies, particularly in outpatient settings.
Beyond the Headlines
The guidelines also highlight the importance of personalized medicine, as they recommend different BP targets based on individual patient conditions, such as the presence of bilateral carotid stenosis or major artery occlusion. This approach underscores the need for healthcare systems to adopt more tailored treatment plans that consider the unique needs of each patient. Furthermore, the guidelines may influence policy decisions regarding healthcare funding and resource allocation, particularly in stroke care units.