What's Happening?
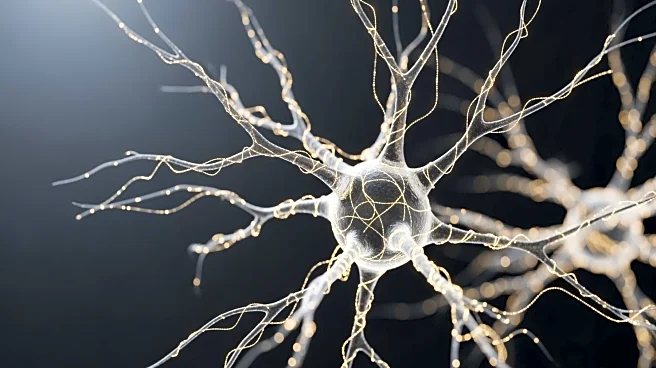
The Hemopatch Sealing Hemostat, a collagen pad used for hemostasis and sealing in neurosurgery, has received a new publication in Frontiers in Surgery. The publication confirms its effectiveness in reducing postoperative complications such as cerebrospinal fluid (CSF) leakage and bleeding, which can lead to infections, reoperations, and prolonged hospital stays. The Hemopatch has been launched in Europe, New Zealand, and Australia, and is now gaining recognition for its ability to achieve watertight dural closure and excellent tissue adherence. The device is indicated for use in various soft tissues and is particularly beneficial when conventional surgical techniques are insufficient.
Why It's Important?
The Hemopatch Sealing Hemostat represents a significant advancement in neurosurgery, offering a reliable solution for managing bleeding and fluid leakage during and after surgery. Its use can potentially reduce healthcare costs by minimizing complications and the need for additional interventions. The device's effectiveness in achieving hemostasis and sealing could lead to improved patient outcomes and shorter hospital stays, benefiting both patients and healthcare providers. As neurosurgery continues to evolve, innovations like the Hemopatch are crucial for enhancing surgical techniques and patient care.
What's Next?
The continued evaluation and publication of clinical data on the Hemopatch may lead to broader adoption in neurosurgical practices worldwide. As more healthcare professionals become aware of its benefits, the Hemopatch could become a standard tool in neurosurgery, influencing surgical protocols and training. Further research and development may expand its applications to other surgical specialties, enhancing its utility and impact on patient care.
Beyond the Headlines
The development and use of the Hemopatch raise ethical considerations regarding the accessibility and affordability of advanced medical devices. Ensuring that such innovations are available to all patients, regardless of geographic or economic barriers, is a critical aspect of healthcare equity. The device also highlights the importance of ongoing research and collaboration among international medical communities to improve surgical outcomes.