What's Happening?
Researchers have successfully reprogrammed human stomach cells to produce insulin, potentially revolutionizing treatment for type 1 diabetes. The study, led by Xiaofeng Huang, PhD, of Weill Cornell Medicine
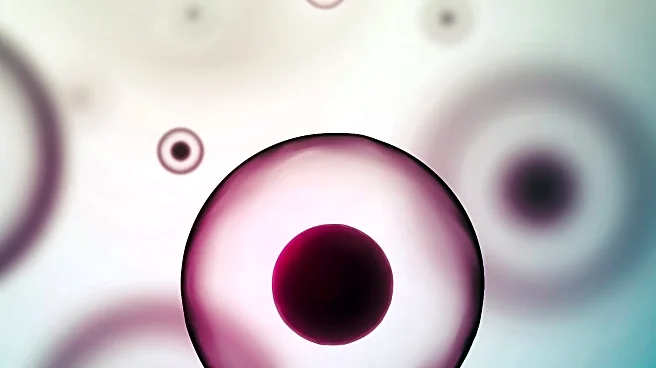
and Qing Xia, MD, PhD, of Peking University, demonstrated that human gastric tissue can be transformed into insulin-producing cells using specific genetic factors. This breakthrough builds on previous findings in mice and marks the first time such conversion has been achieved in human-derived tissues. The research involved engineering human gastric organoids, which are three-dimensional structures derived from human embryonic stem cells. These organoids were transplanted into immunodeficient mice, where they matured and began expressing insulin upon activation of a genetic switch. The engineered cells significantly improved blood glucose control in diabetic mice, suggesting the feasibility of inducing insulin-secreting cells directly in the human stomach.
Why It's Important?
This development could significantly impact the treatment of type 1 diabetes, which currently relies on lifelong insulin administration or experimental stem cell-derived islet transplants. These existing treatments have limitations, including immune rejection and limited donor availability. By enabling the production of insulin-secreting cells from a patient's own stomach tissue, this approach could bypass donor shortages and reduce the risks associated with systemic immunosuppression. If successful, it could lead to a functional cure for type 1 diabetes, improving the quality of life for millions of people worldwide. The ability to reprogram a patient's own cells to produce insulin directly within the body represents a major advancement in regenerative medicine.
What's Next?
While the findings are promising, extensive safety and efficacy testing is required before this approach can be applied clinically. The study used a single embryonic stem cell line, and the induced cells did not yet organize into islet-like structures. Additionally, long-term hyperglycemia was not maintained at a steady level in the transplanted mice. Researchers will need to address these limitations and conduct further studies to ensure the approach is safe and effective for human use. If successful, this method could transform diabetes treatment and pave the way for other regenerative therapies.
Beyond the Headlines
The ethical implications of using embryonic stem cells and genetic reprogramming in medical treatments are significant. This approach raises questions about the long-term effects of genetic modifications and the potential for unintended consequences. Additionally, the development of autologous cell-based therapies could shift the focus of diabetes treatment from managing symptoms to addressing the root cause of the disease. This could lead to broader changes in healthcare practices and policies, emphasizing personalized medicine and regenerative therapies.