What's Happening?
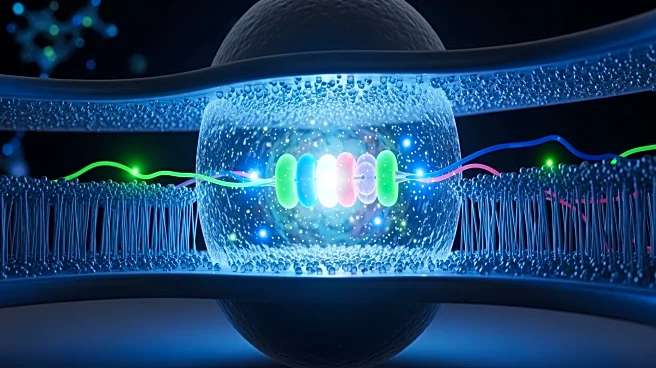
A recent study has highlighted the role of the CXCR4 chemokine receptor in enhancing the memory and persistence of CAR-T cells, which are used in targeting acute myeloid leukemia (AML). The research, conducted on AML patients, demonstrated that CXCR4 expression
is enriched in memory T cell populations, which are crucial for durable anti-leukemic immunity. The study utilized Cytometry by Time-of-Flight (CyTOF) to analyze T cells from patients in remission or relapse, revealing that CXCR4 expression correlates with memory markers and is associated with improved T cell survival and function. The findings suggest that engineering CAR-T cells to express CXCR4 could enhance their memory and antitumor capabilities, offering a potential strategy to improve the efficacy of CAR-T cell therapies against AML.
Why It's Important?
The significance of this study lies in its potential to improve CAR-T cell therapies, which are a promising treatment for various cancers, including AML. By enhancing the memory and persistence of CAR-T cells, the engineered CXCR4 expression could lead to more effective and long-lasting cancer treatments. This advancement could reduce the likelihood of cancer relapse and improve patient outcomes. The study also addresses the challenge of targeting AML cells without affecting normal hematopoietic cells, which is a critical concern in developing safe and effective cancer therapies. The findings could pave the way for more targeted and less toxic cancer treatments, benefiting both patients and healthcare providers.
What's Next?
Future research will likely focus on further validating the role of CXCR4 in enhancing CAR-T cell memory and persistence in clinical settings. Clinical trials may be conducted to test the efficacy and safety of CXCR4-engineered CAR-T cells in AML patients. Additionally, researchers may explore the application of this approach to other types of cancer, potentially broadening the impact of this discovery. The development of off-the-shelf CAR-T products using cord blood-derived T cells, as suggested by the study, could also be a focus, offering a more accessible and scalable treatment option.