What's Happening?
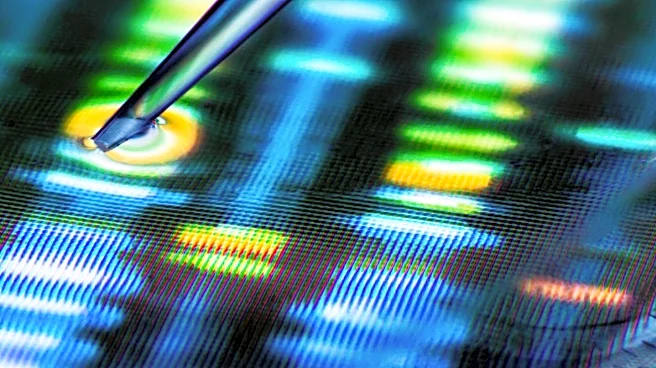
Researchers have utilized Oxford Nanopore Technologies sequencing to analyze plasma cell-free DNA (cfDNA) from critically ill patients, enabling simultaneous detection of tissue injury and pathogens. This method captures methylation marks for tissue-of-origin
inference and microbial cfDNA, providing insights into organ-specific injury and immune activation. The study demonstrated correlations between cfDNA concentrations and clinical markers, such as ALT and troponin T, in patients with organ failure and infections. The technique offers a dual diagnostic approach, potentially enhancing personalized clinical decision-making in intensive care settings.
Why It's Important?
This advancement in nanopore sequencing is crucial for improving diagnostics in intensive care units, where rapid and accurate detection of organ injury and infections can significantly impact patient outcomes. By providing real-time insights into tissue-specific damage and microbial presence, this method could lead to more targeted and effective treatments, reducing mortality rates among critically ill patients. The ability to perform dual host-pathogen diagnostics at bedside-relevant sequencing depths represents a significant step forward in personalized medicine.
What's Next?
Future research will focus on validating these findings in larger patient cohorts and optimizing sequencing methods to enhance sensitivity and specificity. The development of scalable, real-time diagnostics could revolutionize intensive care practices, with potential applications in dynamic risk stratification and personalized treatment plans. Stakeholders in healthcare and biotechnology will likely explore collaborations to advance these technologies for broader clinical use.