What's Happening?
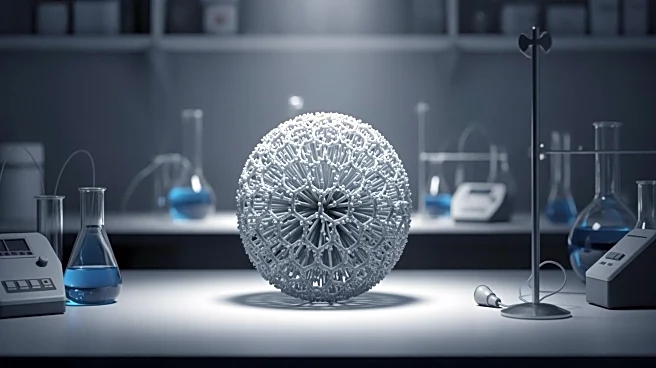
A recent study published in Nature has introduced a 3D spheroid model aimed at improving the delivery of nanocarrier-based drugs to solid tumors, specifically pancreatic ductal adenocarcinoma (PDAC). The research utilized two distinct PDAC cell lines,
PANC-1 and BxPC-3, co-cultured with pancreatic stellate cells to better mimic the tumor microenvironment. The study highlights the challenges of drug penetration in solid tumors and the potential of 3D models to overcome these barriers. The spheroids were developed using low-attachment plates and supplemented with Matrigel to enhance their structural integrity, allowing for a more accurate representation of tumor dynamics and drug resistance.
Why It's Important?
This development is significant as it addresses the limitations of traditional 2D cell cultures in cancer research, which often fail to replicate the complex environment of solid tumors. The 3D spheroid model offers a more realistic platform for testing drug efficacy and penetration, potentially leading to more effective cancer treatments. By simulating the tumor microenvironment, researchers can better understand the mechanisms of drug resistance and identify new therapeutic targets. This model could accelerate the development of nanocarrier-based therapies, offering hope for improved outcomes in cancer treatment.
What's Next?
The study suggests further exploration of the 3D spheroid model in other cancer types beyond PDAC, such as lung adenocarcinoma. Researchers plan to use this model to test the efficacy of various nanocarrier formulations and their ability to penetrate tumor tissues. The model's adaptability to different cancer types could lead to its widespread application in pre-clinical drug testing, potentially streamlining the development of new cancer therapies. Future studies may focus on optimizing the model for high-throughput screening and exploring its use in personalized medicine.
Beyond the Headlines
The introduction of this 3D spheroid model could have broader implications for cancer research, particularly in understanding the role of the tumor microenvironment in drug resistance. It highlights the importance of developing more physiologically relevant models to study cancer biology and treatment. The model's ability to mimic the complex interactions within tumors could lead to new insights into cancer progression and metastasis, ultimately informing the development of more targeted and effective therapies.