What's Happening?
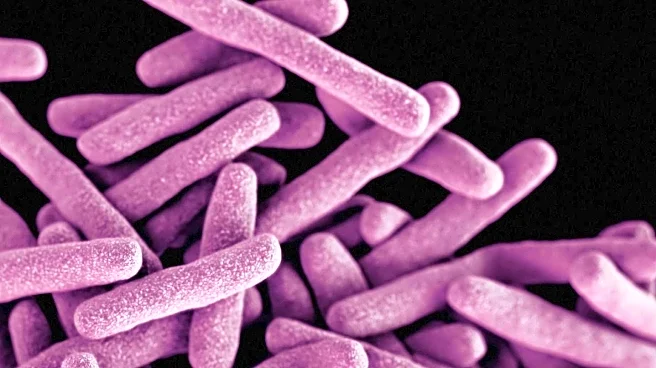
The United States is experiencing a significant increase in cases of carbapenem-resistant Enterobacteriaceae (CRE), known as 'nightmare bacteria.' According to a report by the Centers for Disease Control and Prevention, infection rates have risen nearly 70% from 2019 to 2023. The surge is primarily driven by bacteria with the NDM gene, which are resistant to most antibiotics. The rise in cases is attributed to increased antibiotic use during the COVID-19 pandemic, which has contributed to greater drug resistance. The CDC's data, drawn from 29 states, indicates that many cases remain unreported, suggesting the actual number of infections may be higher.
Why It's Important?
The increase in drug-resistant bacterial infections poses a serious threat to public health, as it complicates treatment options and increases the risk of widespread outbreaks. The limited effectiveness of existing antibiotics against these infections highlights the urgent need for new treatments and better antibiotic stewardship. Hospitals and healthcare providers face challenges in managing these infections, which could lead to higher healthcare costs and strain on medical resources. The situation underscores the importance of continued research and investment in combating antimicrobial resistance.
What's Next?
Healthcare authorities are expected to enhance surveillance and reporting of drug-resistant infections to better understand and address the issue. There may be increased efforts to develop new antibiotics and alternative treatments. Public health campaigns will likely focus on educating the public and healthcare professionals about responsible antibiotic use to prevent further resistance. Policymakers may consider regulatory measures to ensure more comprehensive testing and reporting across all states.
Beyond the Headlines
The rise of 'nightmare bacteria' raises ethical and legal questions about the responsibility of pharmaceutical companies and healthcare providers in preventing antibiotic misuse. It also highlights the need for global cooperation in addressing antimicrobial resistance, as bacteria can easily spread across borders. The situation may prompt discussions on the balance between innovation in drug development and the accessibility of affordable treatments for all populations.