What's Happening?
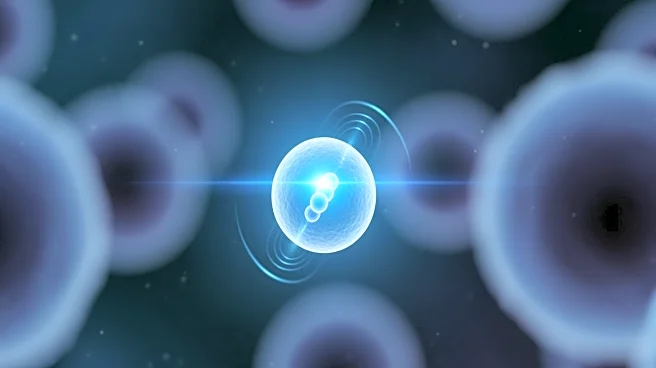
A research team from KAIST, led by Professor Ji-Ho Park of the Department of Bio and Brain Engineering, has developed a novel therapeutic approach that reprograms immune cells within tumors to become anticancer
cell therapies. This method involves the use of lipid nanoparticles to deliver mRNA and immunostimulants directly into tumors, converting existing macrophages into 'CAR-macrophages.' These engineered immune cells are capable of recognizing and attacking cancer cells, while also activating surrounding immune cells to enhance the anticancer response. This approach addresses the limitations of traditional CAR-macrophage therapies, which require the extraction and genetic modification of immune cells outside the body, a process that is both costly and time-consuming.
Why It's Important?
This development is significant as it offers a more efficient and potentially more effective method of cancer treatment. By reprogramming immune cells directly within the body, the therapy could reduce the time and cost associated with current CAR-macrophage treatments. This method also overcomes the challenge of the immunosuppressive tumor environment, which has limited the effectiveness of existing therapies. The ability to activate a systemic immune response could lead to broader applications in treating various types of solid tumors, potentially improving outcomes for patients with cancers that are difficult to treat with current methods.
What's Next?
The research team plans to further investigate the therapeutic potential of this approach in clinical settings. Future studies will likely focus on optimizing the delivery system and assessing the long-term efficacy and safety of the therapy in human patients. If successful, this could pave the way for new cancer treatment protocols that are less invasive and more accessible to a wider range of patients. The development also opens up possibilities for collaboration with pharmaceutical companies to bring this innovative therapy to market.
Beyond the Headlines
This advancement in cancer treatment highlights the growing importance of bioengineering in medical research. The ability to manipulate immune cells within the body represents a significant shift in how cancer therapies are developed and administered. It also raises ethical considerations regarding the manipulation of human cells and the potential long-term effects of such treatments. As this technology progresses, it will be crucial to address these ethical concerns and ensure that the benefits of the therapy are accessible to all patients in need.