What is the story about?
What's Happening?
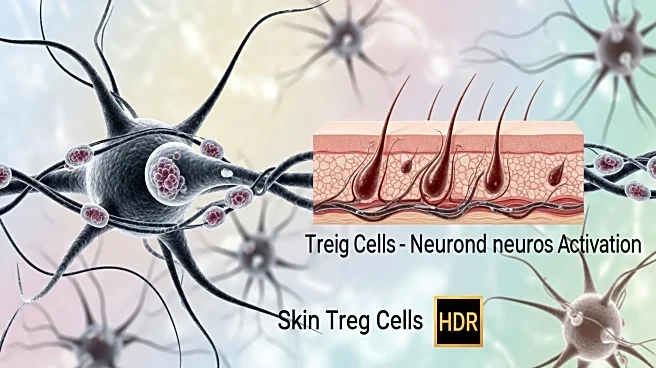
Recent research has uncovered a novel function of regulatory T (Treg) cells in the skin, demonstrating their ability to directly regulate neuronal activity through the production of the opioid enkephalin. The study, conducted by Mendoza et al., utilized gene expression datasets to identify the gene Penk, which encodes the precursor proenkephalin, as being significantly upregulated in a subset of activated Treg cells. These Penk-expressing Treg cells were found to be prevalent in the skin, particularly near axons, and their presence increased following IMQ treatment. The study also revealed that these cells express Ccr2, potentially facilitating their colocalization with CCL2-producing axons. The findings suggest that Treg cells can modulate sensory neuron activation by reducing proinflammatory mediators, thereby maintaining homeostasis in response to various stimuli.
Why It's Important?
This discovery is significant as it expands the understanding of the immune system's role in regulating neuronal activity, particularly in barrier tissues like the skin. By identifying the direct influence of Treg cells on neurons, the research opens new avenues for exploring therapeutic strategies for conditions involving sensory neuron dysregulation, such as chronic pain or inflammatory skin disorders. The ability of Treg cells to produce enkephalin and modulate neuronal activity could lead to innovative treatments that harness the body's own regulatory mechanisms to alleviate symptoms associated with these conditions. Furthermore, understanding the interaction between immune cells and neurons could have broader implications for neuroimmune communication and its role in health and disease.
What's Next?
Future research may focus on further elucidating the mechanisms by which Treg cells influence neuronal activity and exploring the potential for targeting these pathways in therapeutic applications. Investigations into the role of glucocorticoid receptor signaling in facilitating Penk expression could provide insights into how stress responses are managed at the cellular level. Additionally, studies might explore the implications of these findings in other barrier tissues and their potential impact on systemic immune responses. The development of treatments based on these insights could revolutionize approaches to managing inflammatory and neurodegenerative conditions.
Beyond the Headlines
The study highlights the complex interplay between the immune system and the nervous system, suggesting that immune cells may have broader roles in regulating neuronal functions than previously understood. This could lead to a paradigm shift in how researchers approach the study of neuroimmune interactions, potentially influencing fields such as immunology, neurology, and dermatology. The ethical considerations of manipulating immune responses to affect neuronal activity will also need to be addressed as research progresses.