What's Happening?
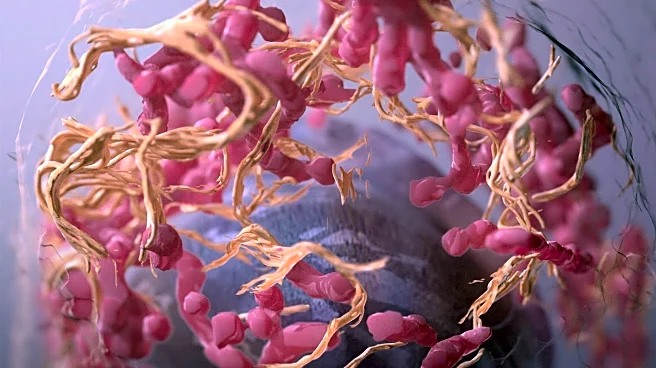
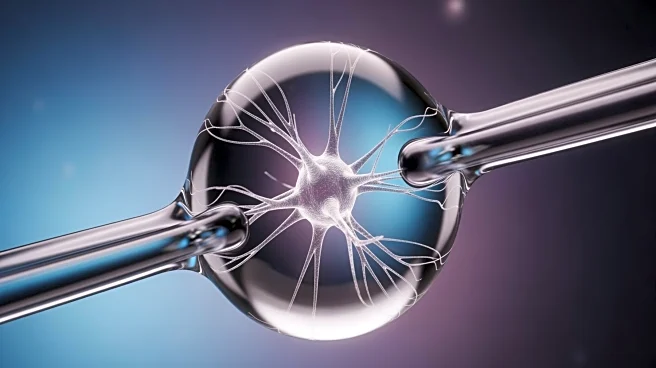
A recent study conducted by researchers at the University of Cambridge has revealed that chronic stress can lead to the migration of immune cells, specifically neutrophils, from the skull's bone marrow to the brain's protective membranes, contributing to depressive symptoms. The study, which involved experiments on mice, found that blocking a specific immune pathway, type I interferon signaling, reduced the presence of these cells in the brain and improved mood-related behaviors. This discovery highlights the role of inflammation in mood disorders and suggests potential new treatments targeting the immune system rather than traditional brain chemistry approaches.
Why It's Important?
The findings of this study are significant as they offer a new perspective on the treatment of depression, particularly for patients who do not respond to conventional antidepressants. By identifying the immune system's involvement in mood disorders, researchers can develop targeted therapies that address inflammation-related depression. This could lead to more effective treatments for a substantial portion of the population suffering from mood disorders. Additionally, the study provides insights into the overlap between depression and other neurological conditions, such as stroke and Alzheimer's disease, potentially paving the way for comprehensive treatment strategies.
What's Next?
The study opens avenues for further research into immune-targeted therapies for depression. Researchers may explore clinical trials to test new drugs that specifically target inflammation in the brain. Additionally, the identification of biomarkers related to inflammation could help tailor treatments to individuals whose depression is linked to immune system activity. This personalized approach could improve the success rates of clinical trials and lead to more effective interventions for mood disorders.
Beyond the Headlines
The study's findings also suggest a potential link between chronic stress-induced inflammation and long-term neurological damage, which could explain why depression is a risk factor for dementia. Understanding the role of neutrophils in brain inflammation may provide insights into preventing or mitigating cognitive decline associated with mood disorders.